Final ID: MP1275
Primary non-adherence and patterns of underutilization of guideline-directed medical therapy following hospitalizations for myocardial infarction
Guideline-directed medical therapy (GDMT) following a myocardial infarction (MI) is crucial for secondary prevention. Prescription of GDMT is emphasized at hospital discharge, but GDMT adherence and persistence following the initial prescription are often overlooked.
Methods
Retrospective cohort study of electronic health records from a 40-hospital US health system. We included adults hospitalized for MI and discharged home between 1/2018-9/2022. We measured GDMT as treatment with beta-blockers (BBs), renin-angiotensin-aldosterone system inhibitors (RAASis), high-intensity statins, and P2Y12 inhibitors. We categorized use of each GDMT class as continuation (fills prior to hospitalization), initiation (a new fill within 7 days of discharge), or primary non-adherence (new prescription at discharge, but absence of a fill). Among continuers and initiators, we defined secondary adherence at 12 months as proportion of days covered (PDC) ≥80% and persistence as continuous days’ supply at 12 months with 90 day grace periods. We tested differences in persistence by continuation vs initiation and by STEMI vs NSTEMI using log-rank tests.
Results
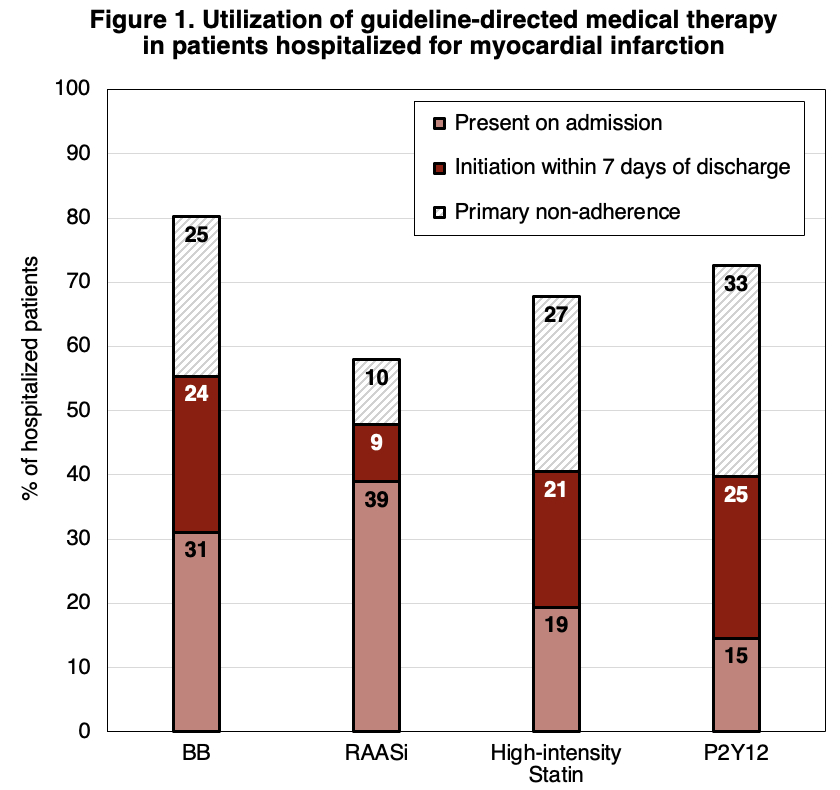
The cohort included 5265 MI hospitalizations (age 68 (IQR 77-60) years, 39% female, 91% White, 7% Black, 75% NSTEMI). Among those without use prior to admission, 71%, 31%, 60%, and 68% of patients were newly prescribed BBs, RAASis, statins, and P2Y12s, respectively, at discharge (Figure 1).
However, 54% of new prescriptions for GDMT were unfilled by 7 days post-discharge, indicating primary non-adherence. In total, only 55%, 48% 41%, and 40% of patients continued or initiated BBs, RAASis, statins, and P2Y12s at discharge, respectively. As a result, 14% of patients received all four GDMT medications at discharge.
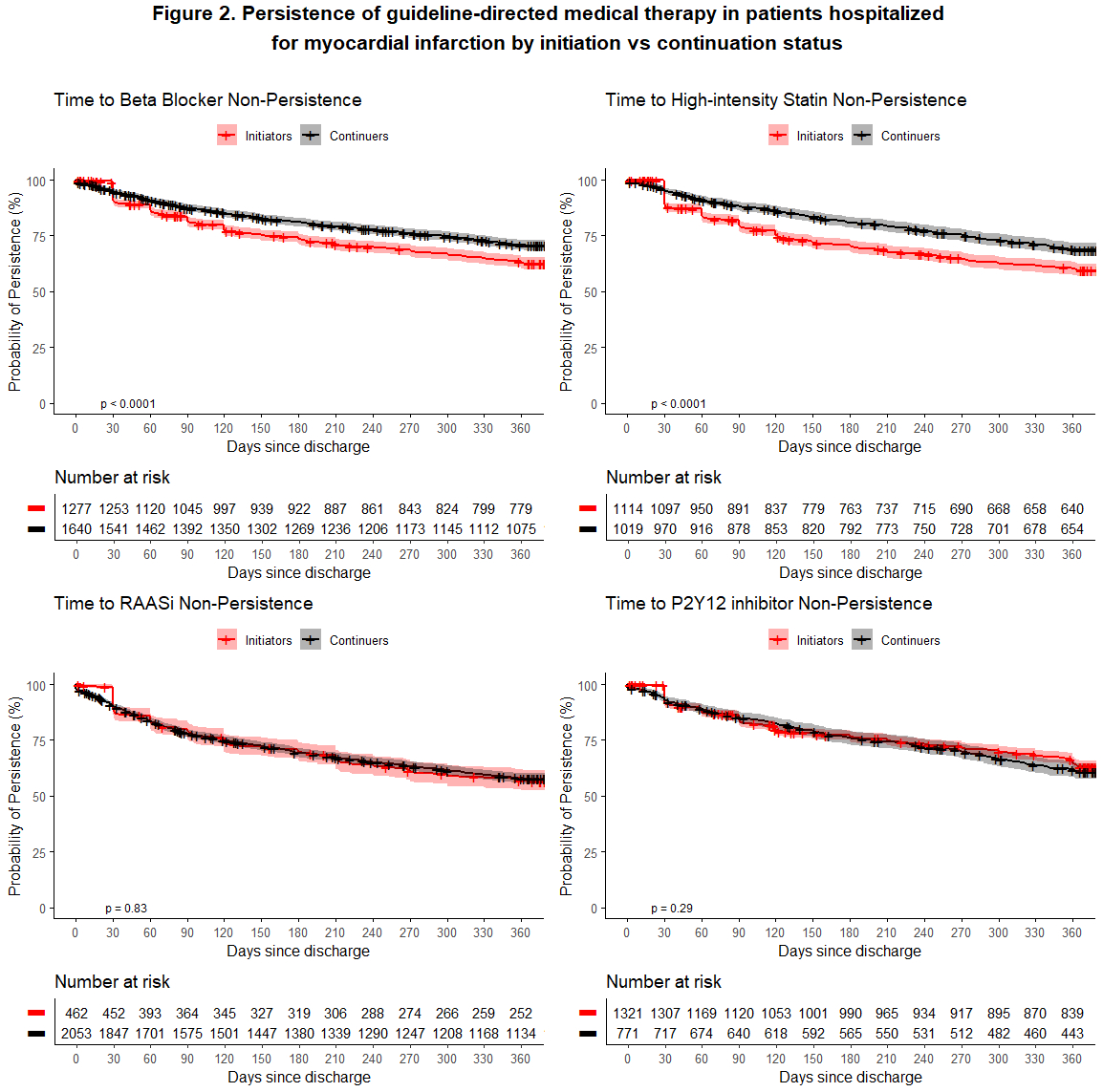
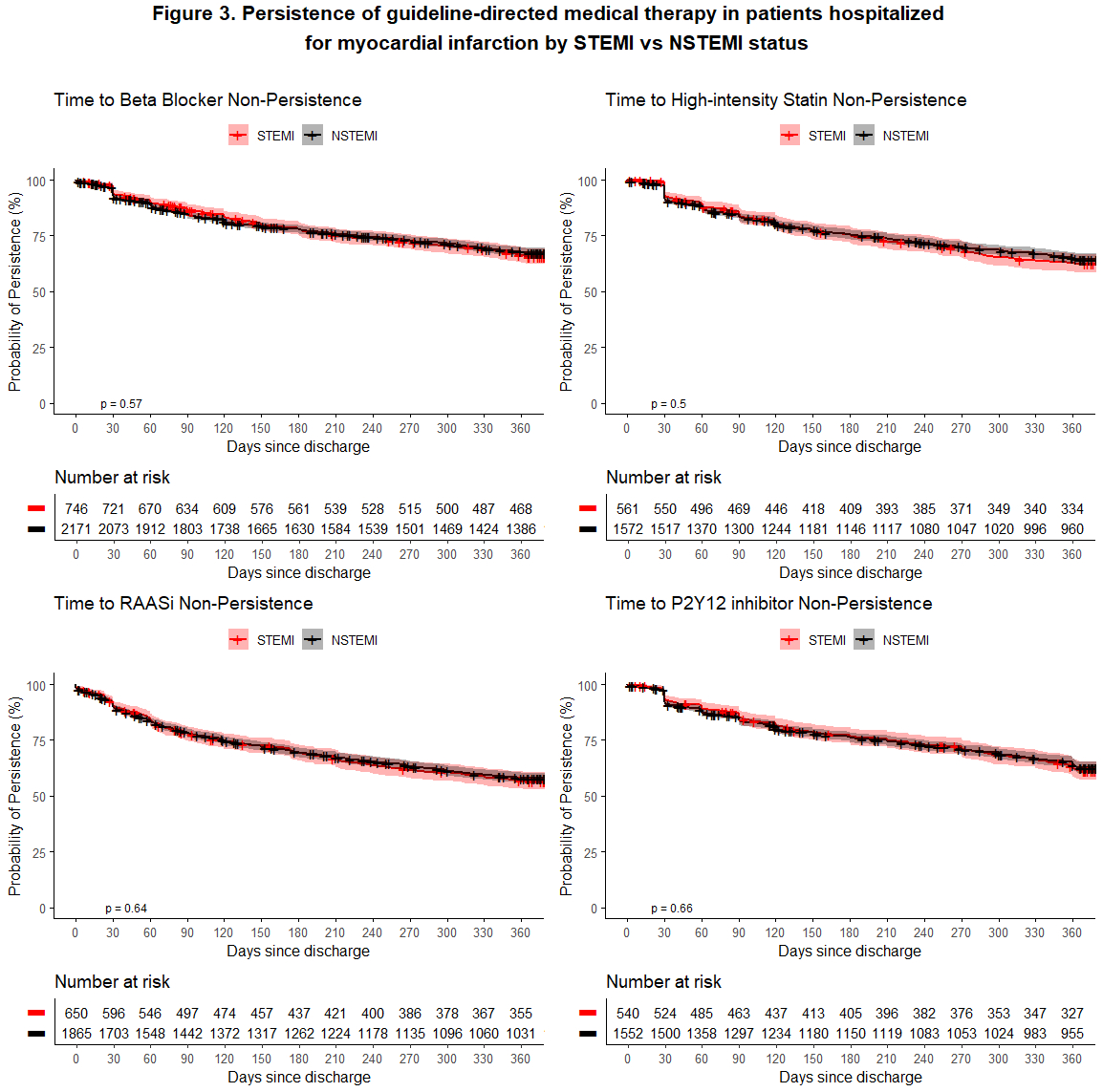
At 12 months post-discharge, 58% were adherent and 48% were persistent to all discharge GDMT medications. Differences in persistence of BBs and statins were observed by initiation status, but not for RAASis or P2Y12s (Figure 2). There were no significant differences in GDMT persistence between patients with STEMI vs NSTEMI (Figure 3).
Conclusions
In our cohort, over half of GDMT prescriptions for secondary prevention following an MI hospitalization went unfilled, and only half of patients were adherent or persistent to GDMT in the year following an MI hospitalization. These results emphasize the need for interventions to support medication adherence following transitions in the post-discharge period.
More abstracts on this topic:
Moon Jungyeon, Chiang Erin, Rodriguez Albert, Ozaki Aya, Lee Douglas, Mody Freny, Udell Jacob, Jackevicius Cynthia
Anticoagulation versus antiplatelet for secondary prevention in embolic stroke of undetermined source: The Cardiac Abnormalities in Stroke Prevention and Risk of Recurrence StudySiegler James, Aboul-nour Hassan, De Havenon Adam, Culbertson Collin, Melkumova Emiliya, Jillella Dinesh, Dumitrascu Oana, Doolittle Charles, Yahnke Ian, Sathya Anvitha, Brown Samantha, Penckofer Mary, Kang Jieun, Bowman Anna, Brorson James, Shahrivari Mahan, Elangovan Cheran, Sloane Kelly, Alvi Muhammad, Krishnaiah Balaji, Kam Wayneho, Farooqui Mudassir, Badillo Goicoechea Elena, Nahab Fadi, Rojas-soto Diana, Sharma Richa, Thottempudi Neeharika, Nedelcu Simona, Smith Matthew, Herpich Franziska, Glover Patrick, Chahien Dalia, Sehgal Siddharth, Eklund Kelsey, Liebeskind David, Linares Guillermo, Daniel Jean-philippe, Al Kasab Sami, Singh Eesha, D'souza Marissa, Gaudio Elizabeth, Aziz Yasmin, Yaghi Shadi, Salehi Omran Setareh, Stretz Christoph, Thon Jesse, Lineback Christina, Khasiyev Farid, Kerrigan Deborah, Ali Hamid