Final ID: MP1027
Impact of mavacamten on the rates of hospitalization and emergency room (ER) visits in patients with obstructive hypertrophic cardiomyopathy (HCM) in the United States
Abstract Body (Do not enter title and authors here): Background: Mavacamten has been shown to improve functional status and symptoms in patients with obstructive hypertrophic cardiomyopathy (HCM) in both clinical trials and real-world settings. However, data on its impact on healthcare resource utilization remain limited.
Aims: To evaluate changes in hospitalization and emergency room (ER) visit rates following mavacamten treatment in patients with obstructive HCM.
Methods: A self-controlled case series study was conducted using linked claims and electronic health record data from the Optum Market Clarity database. Adults with symptomatic obstructive HCM and ≥1 pharmacy claim for mavacamten (first claim was index) between April 28, 2022, and August 31, 2024, were included. Continuous enrollment was required for ≥1 month both before and after the index. The baseline period was ≤ 12 months pre-index, and follow-up continued until the earliest of mavacamten discontinuation, death, disenrollment, or end of database. Rate ratios (RRs) with 95% confidence intervals (CIs) and p-values were estimated for HCM-related, HCM symptom-related, cardiovascular (CV)-related, and all-cause hospitalizations and ER visits during follow-up vs. baseline using generalized estimating equations. Back pain-related outcomes, anticipated as non-associated with mavacamten, served as negative controls to evaluate unmeasured confounding.
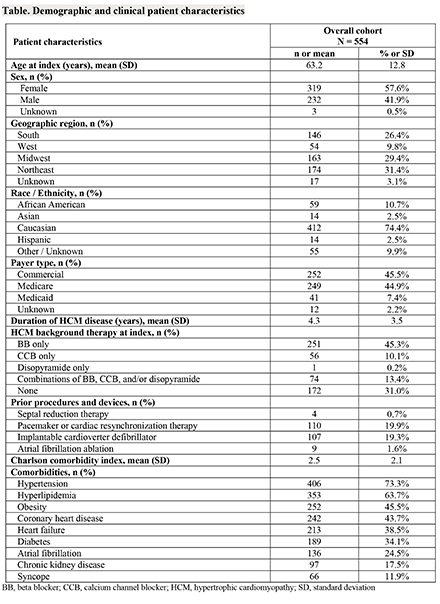
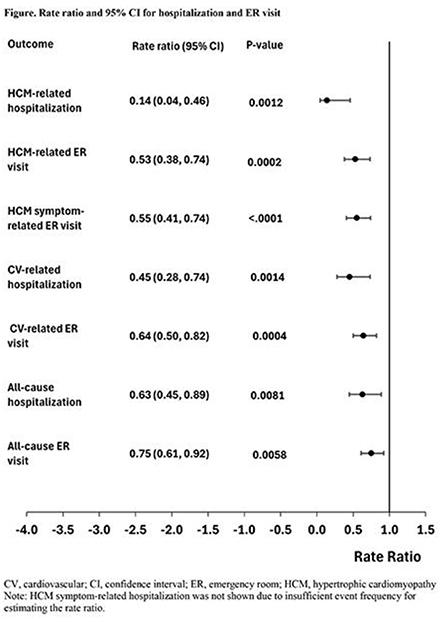
Results: A total of 554 patients (mean ± SD age 63.2 ± 12.8 years; 57.6% female) with a mean ± SD obstructive HCM duration of 4.3 ± 3.5 years were included (Table). Over a mean follow-up of 8.6 ± 6.6 months, hospitalization rates decreased by 86% for HCM-related, 55% for CV-related, and 37% for all-cause events compared to baseline (Figure). ER visit rates declined by 47% for HCM-related, 45% for HCM symptom-related, 36% for CV-related, and 25% for all-cause events. All reductions were statistically significant (p-value < 0.01). RRs for HCM symptom-related and back pain-related hospitalizations were not estimated due to insufficient event frequency. No statistically significant changes were observed for back pain-related ER visits (RR [95% CI] 1.7 [0.7, 3.7], p-value 0.27), suggesting a minimal risk of residual confounding.
Conclusions: Mavacamten treatment was associated with significant reductions in the rates of HCM-related, HCM symptom-related, CV-related, and all-cause hospitalizations and ER visits in patients with obstructive HCM.
Aims: To evaluate changes in hospitalization and emergency room (ER) visit rates following mavacamten treatment in patients with obstructive HCM.
Methods: A self-controlled case series study was conducted using linked claims and electronic health record data from the Optum Market Clarity database. Adults with symptomatic obstructive HCM and ≥1 pharmacy claim for mavacamten (first claim was index) between April 28, 2022, and August 31, 2024, were included. Continuous enrollment was required for ≥1 month both before and after the index. The baseline period was ≤ 12 months pre-index, and follow-up continued until the earliest of mavacamten discontinuation, death, disenrollment, or end of database. Rate ratios (RRs) with 95% confidence intervals (CIs) and p-values were estimated for HCM-related, HCM symptom-related, cardiovascular (CV)-related, and all-cause hospitalizations and ER visits during follow-up vs. baseline using generalized estimating equations. Back pain-related outcomes, anticipated as non-associated with mavacamten, served as negative controls to evaluate unmeasured confounding.
Results: A total of 554 patients (mean ± SD age 63.2 ± 12.8 years; 57.6% female) with a mean ± SD obstructive HCM duration of 4.3 ± 3.5 years were included (Table). Over a mean follow-up of 8.6 ± 6.6 months, hospitalization rates decreased by 86% for HCM-related, 55% for CV-related, and 37% for all-cause events compared to baseline (Figure). ER visit rates declined by 47% for HCM-related, 45% for HCM symptom-related, 36% for CV-related, and 25% for all-cause events. All reductions were statistically significant (p-value < 0.01). RRs for HCM symptom-related and back pain-related hospitalizations were not estimated due to insufficient event frequency. No statistically significant changes were observed for back pain-related ER visits (RR [95% CI] 1.7 [0.7, 3.7], p-value 0.27), suggesting a minimal risk of residual confounding.
Conclusions: Mavacamten treatment was associated with significant reductions in the rates of HCM-related, HCM symptom-related, CV-related, and all-cause hospitalizations and ER visits in patients with obstructive HCM.
More abstracts on this topic:
A Case of Recurrent Acute Coronary Syndrome and Cardiogenic Shock due to Apolipoprotein A-IV Amyloidosis
Muthukkumar Rashmi, Holmes Taylor, Friede Kevin
A Multicenter Friedreich Ataxia Registry Identifies Posterior Wall Thickness as a Predictor of Major Adverse Cardiac EventsLin Kimberly, Johnson Jonathan, Mccormack Shana, Lynch David, Tate Barbara, Feng Yixuan, Huang Jing, Mercer-rosa Laura, Dedio Anna, Mcsweeney Kara, Fournier Anne, Yoon Grace, Payne Ronald, Cripe Linda, Patel Aarti, Niaz Talha