Final ID: MP848
Prophylactic Left Atrial Appendage Occlusion During Mitral Valve Repair in Patients Without Atrial Fibrillation: A Meta-Analysis with Reconstructed Time-to-Event Data
Abstract Body (Do not enter title and authors here):
Background: Mitral valve repair (MVr) is the standard treatment for degenerative mitral regurgitation and is associated with favorable long-term outcomes. However, postoperative atrial fibrillation (AF) and thromboembolic events remain a concern even in patients without a prior history of AF. Prophylactic left atrial appendage occlusion (LAAO), though typically considered in patients with AF, may offer stroke reduction benefits in this population, yet its role remains debated. We aimed to evaluate the long-term and short-term clinical outcomes of prophylactic LAAO at the time of MVr in patients without prior AF.
Methods: A comprehensive literature search was conducted using PubMed, Scopus, Web of Science, and Cochrane databases up to March 2025. Studies comparing prophylactic LAAO versus no-LAAO in patients undergoing MVr without a history of AF were included. The primary outcome was thromboembolic events, mainly stroke. Individual patient data (IPD) were reconstructed from Kaplan-Meier curves using the "IPDfromKM" R package. A Cox regression model was applied to estimate hazard ratios (HR). Random-effects meta-analysis was used for pooled effect estimates of secondary outcomes, including 30-day mortality, in-hospital stroke, postoperative AF, and length of hospital stay (LOH).
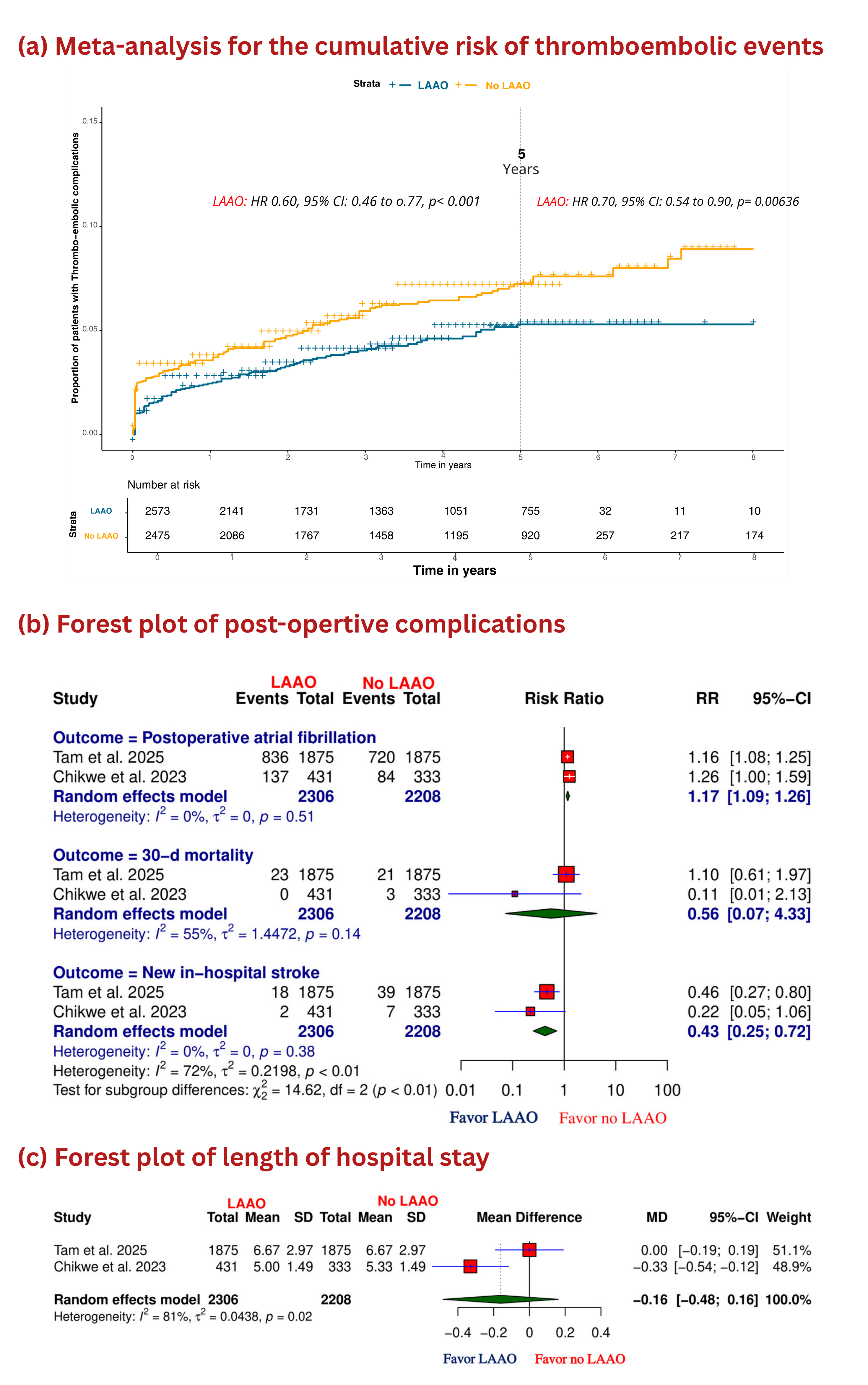
Results: Three retrospective cohort studies were included (n = 5,048; mean age 68 ± 10.3 years; mean follow-up 6 years). Among these, 2,573 patients received LAAO during MVr. Pooled IPD analysis showed significantly lower thromboembolic risk at 5 years (HR 0.60, 95% CI 0.46–0.77, P<0.001) and 8 years (HR 0.70, 95% CI 0.54–0.90, P=0.006). LAAO was associated with reduced in-hospital stroke (RR 0.43, 95% CI 0.25–0.72) with no significant differences in 30-day mortality (RR 0.56, 95% CI 0.07–4.33) or LOH (MD - 0.16 days, 95% CI -0.48–0.16). However, patients undergoing LAAO had higher rates of post-operative AF (RR 1.17, 95% CI 1.09–1.26).
Conclusions: Prophylactic LAAO during MVr in patients without prior AF is associated with a significant reduction in long-term thromboembolic events and in-hospital stroke, without increasing short-term mortality or length of hospitalization. However, the increased risk of postoperative AF highlights the need for individualized decision-making and further large-scale prospective studies.
Background: Mitral valve repair (MVr) is the standard treatment for degenerative mitral regurgitation and is associated with favorable long-term outcomes. However, postoperative atrial fibrillation (AF) and thromboembolic events remain a concern even in patients without a prior history of AF. Prophylactic left atrial appendage occlusion (LAAO), though typically considered in patients with AF, may offer stroke reduction benefits in this population, yet its role remains debated. We aimed to evaluate the long-term and short-term clinical outcomes of prophylactic LAAO at the time of MVr in patients without prior AF.
Methods: A comprehensive literature search was conducted using PubMed, Scopus, Web of Science, and Cochrane databases up to March 2025. Studies comparing prophylactic LAAO versus no-LAAO in patients undergoing MVr without a history of AF were included. The primary outcome was thromboembolic events, mainly stroke. Individual patient data (IPD) were reconstructed from Kaplan-Meier curves using the "IPDfromKM" R package. A Cox regression model was applied to estimate hazard ratios (HR). Random-effects meta-analysis was used for pooled effect estimates of secondary outcomes, including 30-day mortality, in-hospital stroke, postoperative AF, and length of hospital stay (LOH).
Results: Three retrospective cohort studies were included (n = 5,048; mean age 68 ± 10.3 years; mean follow-up 6 years). Among these, 2,573 patients received LAAO during MVr. Pooled IPD analysis showed significantly lower thromboembolic risk at 5 years (HR 0.60, 95% CI 0.46–0.77, P<0.001) and 8 years (HR 0.70, 95% CI 0.54–0.90, P=0.006). LAAO was associated with reduced in-hospital stroke (RR 0.43, 95% CI 0.25–0.72) with no significant differences in 30-day mortality (RR 0.56, 95% CI 0.07–4.33) or LOH (MD - 0.16 days, 95% CI -0.48–0.16). However, patients undergoing LAAO had higher rates of post-operative AF (RR 1.17, 95% CI 1.09–1.26).
Conclusions: Prophylactic LAAO during MVr in patients without prior AF is associated with a significant reduction in long-term thromboembolic events and in-hospital stroke, without increasing short-term mortality or length of hospitalization. However, the increased risk of postoperative AF highlights the need for individualized decision-making and further large-scale prospective studies.
More abstracts on this topic:
“Atrialized” Minimally Invasive Transcatheter Mitral Valve-In-MAC Replacement to Prevent Outflow Tract Obstruction
Steafo Lark, Smielewski Mitchell, Madanat Luai, Bloomingdale Richard, Jabri Ahmad, Gallagher Michael, Birk Vishal, Abbas Amr, Young John, Suri Rakesh
A Royal Flush: A Unique Case of Carcinoid Heart Disease Manifesting in a Rare Fashion as Quadruple Valve InvolvementFraser Elise, Rodriguez L, Mehta Anand, Unai Shinya, Alencherry Ben