Final ID: MP877
Transcatheter vs. Surgical Treatment in Aortic Stenosis with Coronary Artery Disease: A Meta-Analysis of Time-to-Event Data on 162,305 Patients
Abstract Body (Do not enter title and authors here): .Background: The optimal treatment for aortic stenosis (AS) with concomitant coronary artery disease (CAD) is controversial. Our meta-analysis of reconstructed time-to-event data aimed to compare percutaneous coronary intervention (PCI) + transcatheter aortic valve implantation (TAVI) with coronary artery bypass graft (CABG) + surgical aortic valve replacement (SAVR) in AS with CAD.
Methods: We systematically searched four databases (PubMed, Web of Science, Scopus, and Cochrane Library) up to March 2025. Individual patient data (IPD) reconstructed from time-to-event data were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for all-cause mortality. Dichotomous data were analyzed using risk ratios (RR) and with 95% confidence intervals (CI).
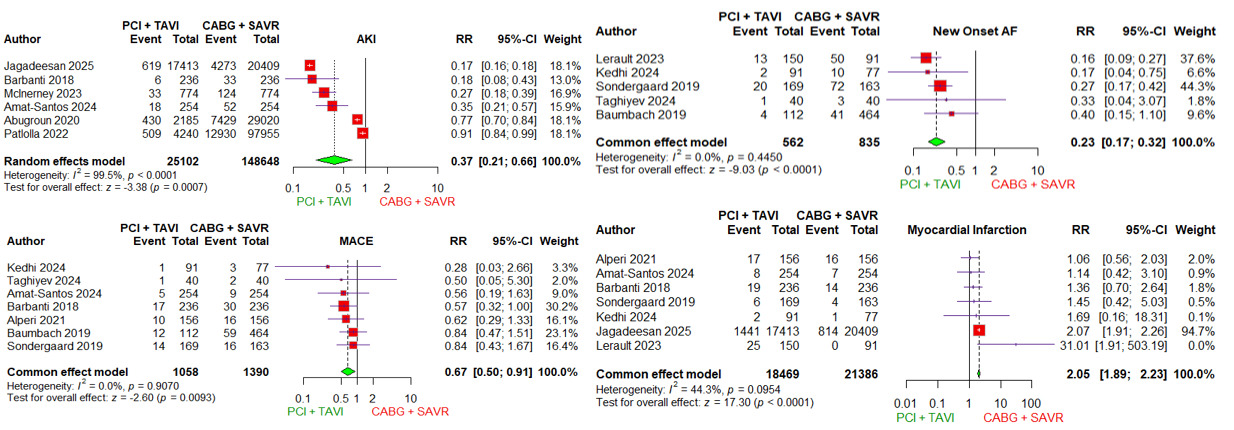
Results: Our study included 15 studies with a total of 162,305 patients. PCI + TAVI significantly increased all-cause mortality compared to CABG + SAVR at 48 months (HR 1.29, 95% CI 1.23–1.35, P<0.001), however, reduced the risk of in-hospital acute kidney injury (AKI) (RR 0.37, 95% CI 0.21–0.66, P=0.0007), and on short term: major adverse cardiac event (MACE) (RR 0.67, 95% CI 0.50–0.91, P=0.0093) and new-onset atrial fibrillation (AF) (RR 0.23, 95% CI 0.17–0.32, P<0.0001). Moreover, PCI + TAVI was associated with an increased risk of myocardial infarction on long-term (RR 2.05, 95% CI 1.89–2.23, P<0.0001).
Conclusions: PCI + TAVI was associated with a significantly higher all-cause mortality and an increased long-term risk of MI compared to the CABG + SAVR. However, it significantly lowered the risk of in-hospital AKI, as well as the short-term incidence of new-onset AF and MACE. However, high quality prospective clinical trials are warranted to reassess current guidelines and refine treatment recommendations.
Methods: We systematically searched four databases (PubMed, Web of Science, Scopus, and Cochrane Library) up to March 2025. Individual patient data (IPD) reconstructed from time-to-event data were used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for all-cause mortality. Dichotomous data were analyzed using risk ratios (RR) and with 95% confidence intervals (CI).
Results: Our study included 15 studies with a total of 162,305 patients. PCI + TAVI significantly increased all-cause mortality compared to CABG + SAVR at 48 months (HR 1.29, 95% CI 1.23–1.35, P<0.001), however, reduced the risk of in-hospital acute kidney injury (AKI) (RR 0.37, 95% CI 0.21–0.66, P=0.0007), and on short term: major adverse cardiac event (MACE) (RR 0.67, 95% CI 0.50–0.91, P=0.0093) and new-onset atrial fibrillation (AF) (RR 0.23, 95% CI 0.17–0.32, P<0.0001). Moreover, PCI + TAVI was associated with an increased risk of myocardial infarction on long-term (RR 2.05, 95% CI 1.89–2.23, P<0.0001).
Conclusions: PCI + TAVI was associated with a significantly higher all-cause mortality and an increased long-term risk of MI compared to the CABG + SAVR. However, it significantly lowered the risk of in-hospital AKI, as well as the short-term incidence of new-onset AF and MACE. However, high quality prospective clinical trials are warranted to reassess current guidelines and refine treatment recommendations.
More abstracts on this topic:
Analysis of Cardiovascular Events in Cancer Survivors: A Comparative Study of Solid Tumors and Hematologic Malignancies at a Tertiary Cardiovascular Center
Amaro Palomo Eder Jonathan, Cortes Flores Claudia Galilea, Diaz Braiana, Araiza Diego, Arias-mendoza Alexandra, Martinez Rios Marco Antonio, Latapi Ruiz Esparza Ximena, Adib Gracia Anna Elisa, Garate Togo Javier, Sierra Lara Martinez Jorge Daniel, Hernandez-pastrana Sarai, Gonzalez Macedo Eder, Santiago Hernández Alberto, Neri Bale Raul Rodrigo
Activin Signaling Inhibition Enhances Cardiac Functional Recovery After Aortic DebandingSingh Anand, Guseh James Sawalla, Xiao Chunyang, Babbs Keith, Seehra Jasbir, Li Haobo, Rosenzweig Anthony