Final ID: MP143
Artificial Intelligence for Diagnosing Low-Gradient Aortic Stenosis Using Echocardiographic Imaging.
Abstract Body (Do not enter title and authors here): Background
Artificial intelligence (AI) may assist in diagnosing the most challenging subtype of aortic stenosis (AS) — low-gradient (LG) AS, characterized by a discordance between the mean aortic gradient and aortic valve area, making accurate assessment of stenosis severity difficult.
Hypothesis
AI models could differentiate between moderate and severe LGAS based solely on automatically-derived echocardiographic parameters, with clinically meaningful accuracy.
Methods
We included transthoracic echocardiograms from 158 out of 174 consecutive patients with suspected LGAS from the National Institute of Cardiology in Warsaw (moderate AS (n=82); severe AS (n=72)). Imaging-derived parameters (left ventricular internal diameter (LVID), interventricular septum thickness (IVS), left ventricular posterior wall thickness (LVPW) and left ventricular ejection fraction (EF) were automatically extracted using two established EchoNet models (Dynamic and LVH), then used to train our model. A semi-automatic approach aditionally incorporated two manually derived Doppler parameters: stroke volume index (SVI) and Doppler velocity index (SVI) - available in 135 patients. Model performance was assessed using stratified cross-validation. Feature importance was evaluated using XGBoost's gain metric, and 95% confidence intervals (CIs) were calculated via bootstrapping.
Results
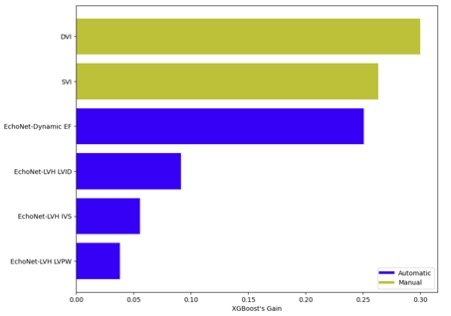
The semi-automatic model, based on six parameters, achieved an AUC of 0.853 (95% CI: 0.788–0.919), the fully automatic model achieved an AUC of 0.660 (95% CI: 0.568–0.752); DeLong’s test, p < 0.0005. (Figure 1) The semi-automatic model subgroup: (1) EchoNet + SVI yielded an AUC of 0.718 (95% CI: 0.632–0.805), (2) EchoNet + DVI yielded an AUC of 0.809 (95% CI: 0.735–0.882), (3) EchoNet + SVI + DVI achieved the highest performance, AUC = 0.853 (95% CI: 0.788–0.919). For fully automatic model applied to all 158 patients using the four imaging-derived parameters, performance improved modestly (AUC = 0.719, 95% CI: 0.640–0.798; p = 0.34). Feature importance analysis identified DVI and SVI as the most predictive parameters, followed by EF, LVID, IVS, and LVPW (Figure 2).
Conclusions.
Our findings indicate that AI models trained exclusively on imaging-based echocardiographic features can effectively distinguish low-gradient severe from moderate aortic stenosis. These models may assist in clinical evaluation, especially in diagnostically challenging cases, potentially minimizing the need for further diagnostic testing.
Artificial intelligence (AI) may assist in diagnosing the most challenging subtype of aortic stenosis (AS) — low-gradient (LG) AS, characterized by a discordance between the mean aortic gradient and aortic valve area, making accurate assessment of stenosis severity difficult.
Hypothesis
AI models could differentiate between moderate and severe LGAS based solely on automatically-derived echocardiographic parameters, with clinically meaningful accuracy.
Methods
We included transthoracic echocardiograms from 158 out of 174 consecutive patients with suspected LGAS from the National Institute of Cardiology in Warsaw (moderate AS (n=82); severe AS (n=72)). Imaging-derived parameters (left ventricular internal diameter (LVID), interventricular septum thickness (IVS), left ventricular posterior wall thickness (LVPW) and left ventricular ejection fraction (EF) were automatically extracted using two established EchoNet models (Dynamic and LVH), then used to train our model. A semi-automatic approach aditionally incorporated two manually derived Doppler parameters: stroke volume index (SVI) and Doppler velocity index (SVI) - available in 135 patients. Model performance was assessed using stratified cross-validation. Feature importance was evaluated using XGBoost's gain metric, and 95% confidence intervals (CIs) were calculated via bootstrapping.
Results
The semi-automatic model, based on six parameters, achieved an AUC of 0.853 (95% CI: 0.788–0.919), the fully automatic model achieved an AUC of 0.660 (95% CI: 0.568–0.752); DeLong’s test, p < 0.0005. (Figure 1) The semi-automatic model subgroup: (1) EchoNet + SVI yielded an AUC of 0.718 (95% CI: 0.632–0.805), (2) EchoNet + DVI yielded an AUC of 0.809 (95% CI: 0.735–0.882), (3) EchoNet + SVI + DVI achieved the highest performance, AUC = 0.853 (95% CI: 0.788–0.919). For fully automatic model applied to all 158 patients using the four imaging-derived parameters, performance improved modestly (AUC = 0.719, 95% CI: 0.640–0.798; p = 0.34). Feature importance analysis identified DVI and SVI as the most predictive parameters, followed by EF, LVID, IVS, and LVPW (Figure 2).
Conclusions.
Our findings indicate that AI models trained exclusively on imaging-based echocardiographic features can effectively distinguish low-gradient severe from moderate aortic stenosis. These models may assist in clinical evaluation, especially in diagnostically challenging cases, potentially minimizing the need for further diagnostic testing.
More abstracts on this topic:
18F-FDG PET/CT Evaluation of Incidental Extracardiac CT Findings on 82Rb-Chloride PET Myocardial Perfusion Imaging
Dhaliwal Jasmeet, David Sthuthi, Puente Cesar, Nandakumar Menon, Sayre James, Zhong Jin, Berenji Gholam, Packard Rene
Aortic Valve Neocuspidization Using Autologous Insertion Of Pulmonary SinusTm: A Proof Of ConceptFaateh Muhammad, Raees Muhammad Aanish, Ahmed Hosam, Almiqlash Bushray, Villalobos Lizardi Jose, Ricci Marco, Ashfaq Awais