Final ID: Sa1005
In-Hospital Outcomes of ECMO Use in Takotsubo Cardiomyopathy with Cardiogenic Shock: A Propensity-Matched Analysis of the National Inpatient Sample
Abstract Body (Do not enter title and authors here): Background:
Takotsubo cardiomyopathy (TCM) is a transient form of left ventricular dysfunction, in which 10% of patients develop cardiogenic shock, requiring advanced circulatory support. ECMO has been used in this patient subpopulation; however, data regarding its efficacy remain limited. The rarity of TCM cases requiring such intervention poses challenges for prospective studies, highlighting the importance of leveraging large-scale datasets to evaluate outcomes.
Research Question:
Does ECMO improve in-hospital outcomes in TCM with cardiogenic shock compared to the non-ECMO group?
Methods:
We conducted a retrospective analysis using the National Inpatient Sample (2016–2022), including adult hospitalizations with TCM complicated by cardiogenic shock. Patients who used an intra-aortic balloon pump were excluded. ECMO use was identified using ICD-10-PCS procedure codes. Propensity score matching (PSM) was performed using 1:1 nearest-neighbor matching with replacement, incorporating age, sex, and Elixhauser comorbidities. Following matching, double adjustment was conducted using survey-weighted logistic and linear regression to evaluate in-hospital mortality and secondary outcomes, including length of stay, total hospital charges, acute kidney injury, and bleeding complications.
Results:
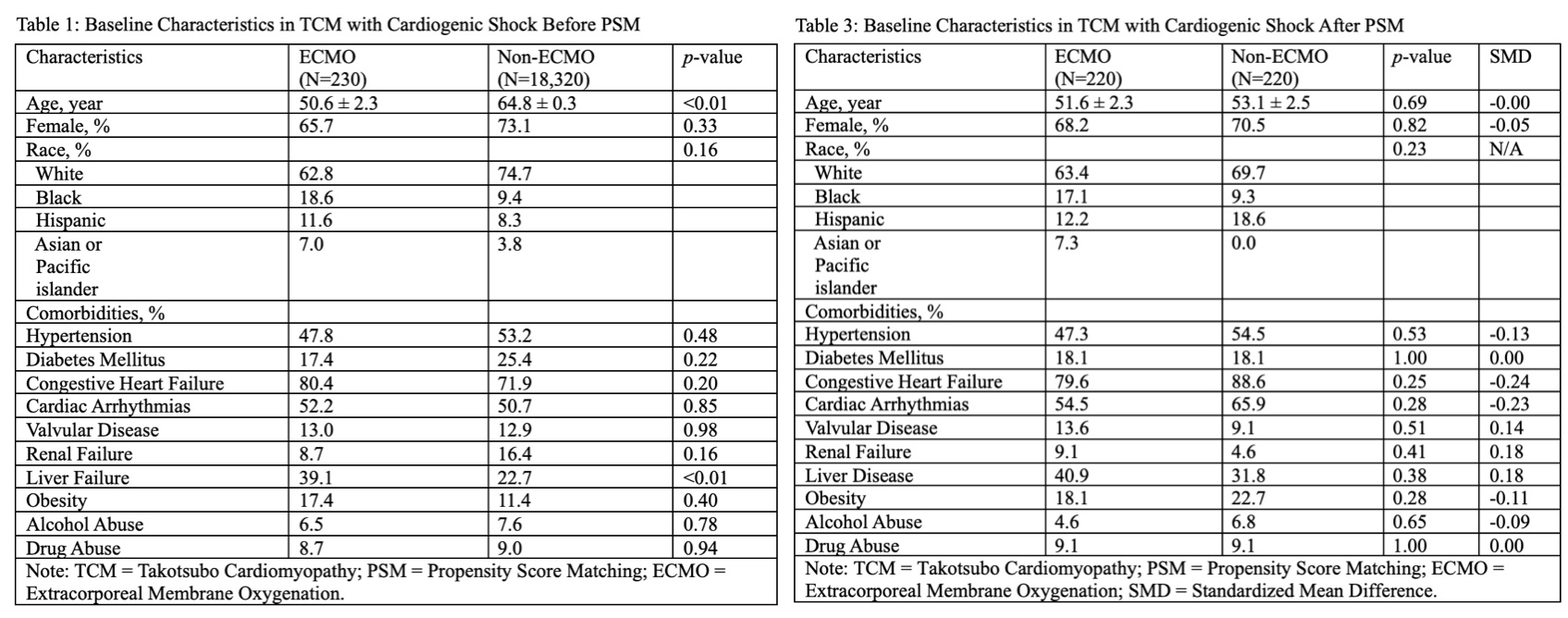
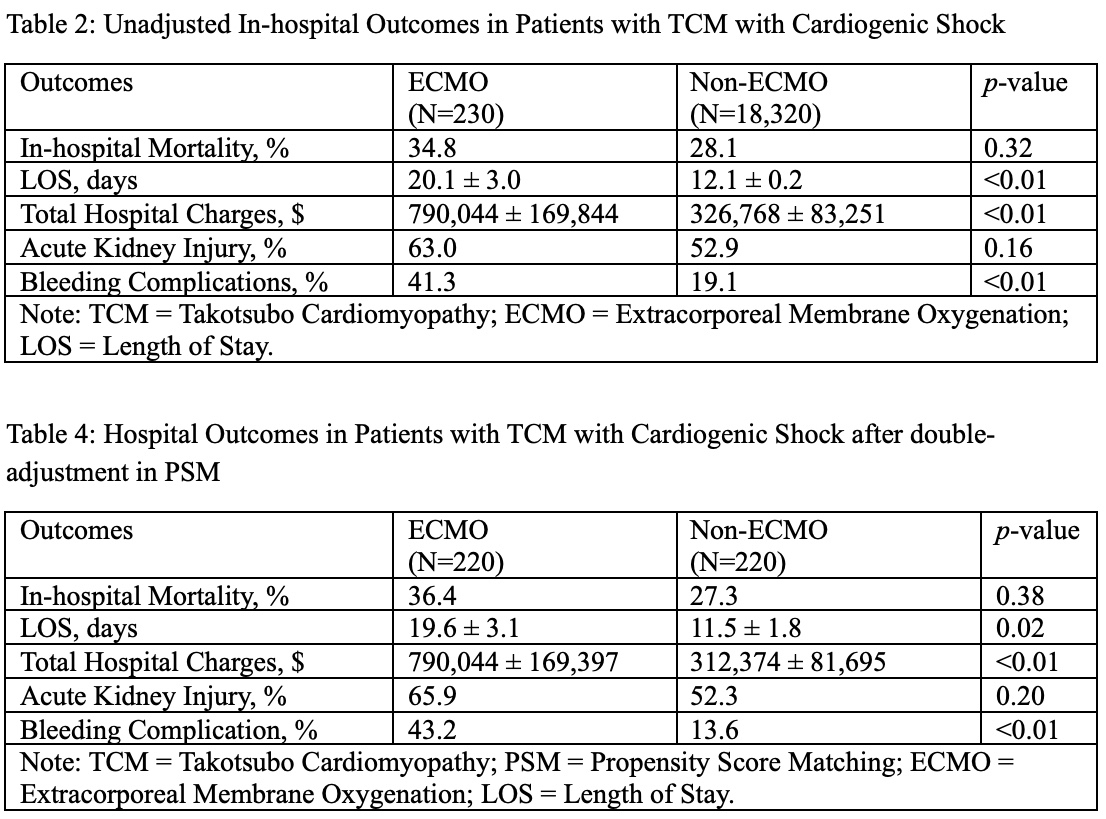
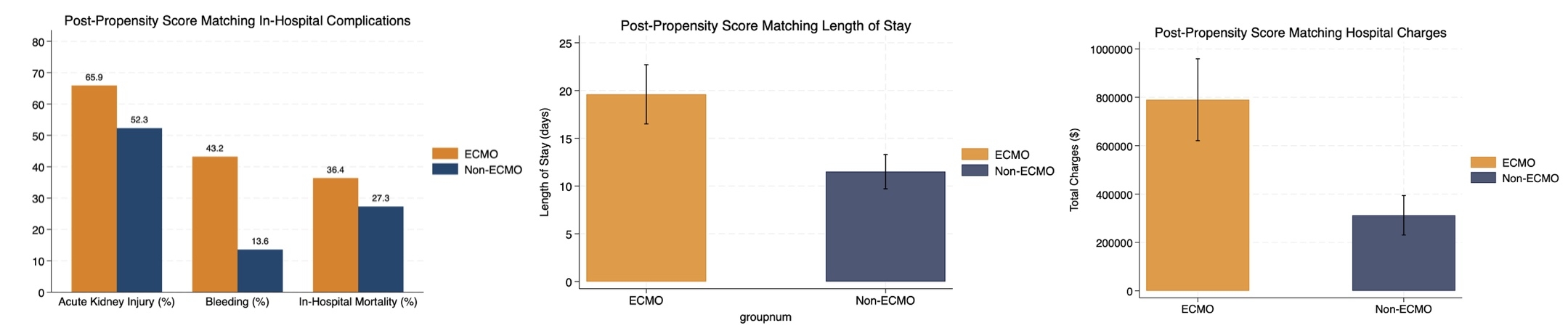
A total of 18,460 weighted admissions were analyzed. Of these, 230 (1.2%) patients received ECMO. Before PSM, ECMO patients were significantly younger than non-ECMO patients (50.6 ± 2.3 vs. 64.8 ± 0.3 years, p<0.01). Comorbidities were comparable between groups, except for liver disease, which was more prevalent in the ECMO group (39.1% vs. 22.7%, p <0.01). After 1:1 PSM (n = 220 per group), in-hospital mortality was higher in the ECMO group (36.4% vs 27.3%, p = 0.38). The ECMO group had significantly longer hospital stay (19.6 ± 3.1 vs. 11.5 ± 1.8 days, p<0.01), higher total hospital charges ($790,044 ± 169,397 vs. $312,374 ± 81,695, p < 0.01), and bleeding complications (43.2% vs. 13.6%, p<0.01). No statistically significant differences were observed in rates of acute kidney injury (65.9% vs. 52.3%, p = 0.20).
Conclusion:
In TCM with cardiogenic shock, ECMO use was not associated with improved in-hospital mortality, but was associated with longer length of stay, higher costs, and higher bleeding complications. These findings underscore the need for careful patient selection and provide valuable real-world evidence in a population where prospective studies are challenging.
Takotsubo cardiomyopathy (TCM) is a transient form of left ventricular dysfunction, in which 10% of patients develop cardiogenic shock, requiring advanced circulatory support. ECMO has been used in this patient subpopulation; however, data regarding its efficacy remain limited. The rarity of TCM cases requiring such intervention poses challenges for prospective studies, highlighting the importance of leveraging large-scale datasets to evaluate outcomes.
Research Question:
Does ECMO improve in-hospital outcomes in TCM with cardiogenic shock compared to the non-ECMO group?
Methods:
We conducted a retrospective analysis using the National Inpatient Sample (2016–2022), including adult hospitalizations with TCM complicated by cardiogenic shock. Patients who used an intra-aortic balloon pump were excluded. ECMO use was identified using ICD-10-PCS procedure codes. Propensity score matching (PSM) was performed using 1:1 nearest-neighbor matching with replacement, incorporating age, sex, and Elixhauser comorbidities. Following matching, double adjustment was conducted using survey-weighted logistic and linear regression to evaluate in-hospital mortality and secondary outcomes, including length of stay, total hospital charges, acute kidney injury, and bleeding complications.
Results:
A total of 18,460 weighted admissions were analyzed. Of these, 230 (1.2%) patients received ECMO. Before PSM, ECMO patients were significantly younger than non-ECMO patients (50.6 ± 2.3 vs. 64.8 ± 0.3 years, p<0.01). Comorbidities were comparable between groups, except for liver disease, which was more prevalent in the ECMO group (39.1% vs. 22.7%, p <0.01). After 1:1 PSM (n = 220 per group), in-hospital mortality was higher in the ECMO group (36.4% vs 27.3%, p = 0.38). The ECMO group had significantly longer hospital stay (19.6 ± 3.1 vs. 11.5 ± 1.8 days, p<0.01), higher total hospital charges ($790,044 ± 169,397 vs. $312,374 ± 81,695, p < 0.01), and bleeding complications (43.2% vs. 13.6%, p<0.01). No statistically significant differences were observed in rates of acute kidney injury (65.9% vs. 52.3%, p = 0.20).
Conclusion:
In TCM with cardiogenic shock, ECMO use was not associated with improved in-hospital mortality, but was associated with longer length of stay, higher costs, and higher bleeding complications. These findings underscore the need for careful patient selection and provide valuable real-world evidence in a population where prospective studies are challenging.
More abstracts on this topic:
Adjunctive pulmonary artery catheter for patients with cardiogenic shock treated with impella: a meta-analysis
Barbosa Lucas, Araujo Beatriz, Aziri Buena, Begic Edin
A Novel Subcellular β-arrestin Biased Allosteric ModulatorAnderson Preston, Rajagopal Sudarshan