Final ID: MP834
Disparities in Cardiac Resynchronization Therapy Utilization Among Women with Heart Failure with Reduced Ejection Fraction and Left Bundle Branch Block: The Impact of Breast Cancer Status
Abstract Body (Do not enter title and authors here): Background:
Cardiac resynchronization therapy (CRT) has been demonstrated to reduce both mortality and morbidity in patients with LBBB. Despite this, CRT remains underutilized in certain populations, particularly among women. Breast cancer generally has a high five-year survival rate of 91% and is commonly treated with cardiotoxic chemotherapy, which increases the risk of HFrEF. Given the risk and potential benefits of CRT, its application in breast cancer patients may be valuable. However, clinical bias or concerns regarding cancer status may contribute to its underuse. This study aims to evaluate disparities in CRT utilization among female patients with breast cancer.
Research Question:
To investigate the disparity in CRT utilization among female patients with breast cancer and HFrEF with LBBB compared to those without.
Methods:
We conducted a cross-sectional study using the National Inpatient Sample (2016-2022) to identify adult female hospitalizations with a diagnosis of HFrEF and LBBB. The history of breast cancer was determined using ICD-10-CM codes. Survey-weighted analyses were used to compare baseline characteristics and outcomes, including CRT use, in-hospital mortality, length of stay, and comorbidities. Logistic regression was performed to adjust for potential confounders.
Results:
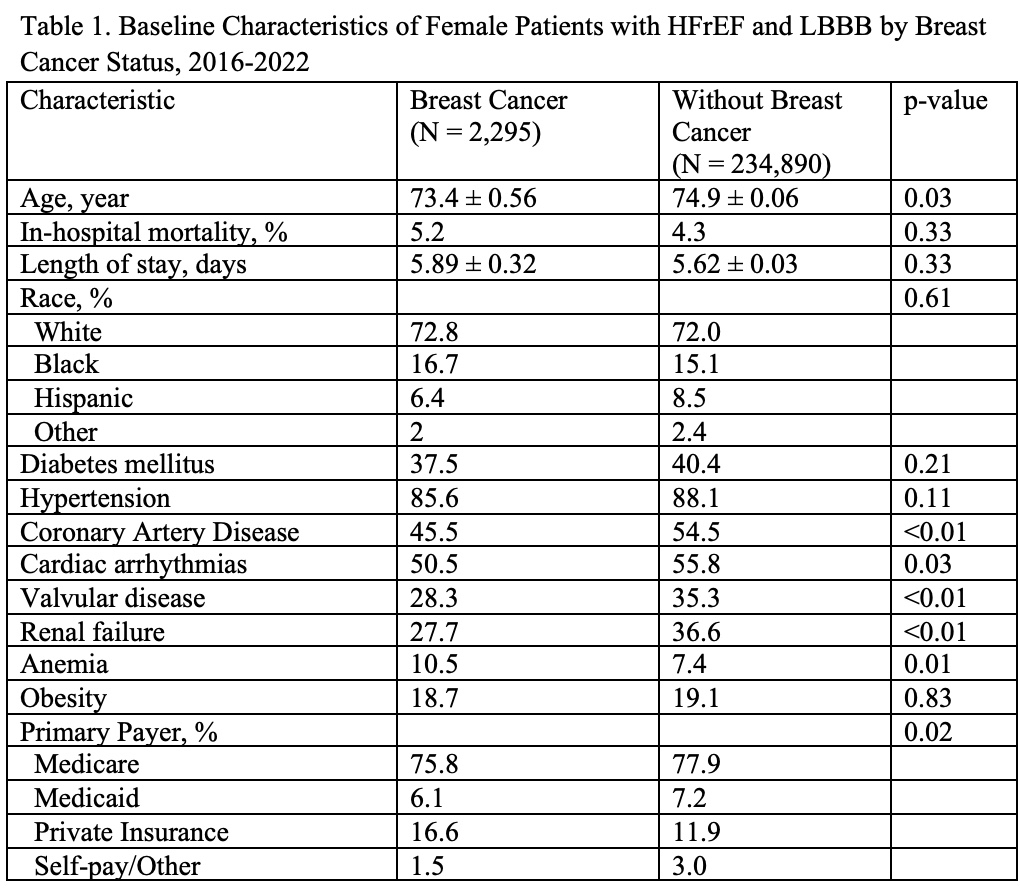
A total of 47,437 adult women with HFrEF and LBBB were included in the analysis. Of these, 2,295 (1.0%) had breast cancer. Compared to non-cancer patients, those with breast cancer were younger (73.4 vs. 74.9 years, p < 0.01), had a lower prevalence of renal failure (27.7% vs. 36.6%, p < 0.01), valvular disease (28.3% vs. 35.3%, p <0.01), and anemia (10.5% vs. 7.4%, p = 0.01). No significant differences were observed in diabetes or obesity between the two groups. In-hospital mortality (5.2% vs. 4.3%, p = 0.33), length of stay (5.9 vs. 5.6 days), and arrhythmia burden (50.5% vs. 55.8%) were comparable between groups.
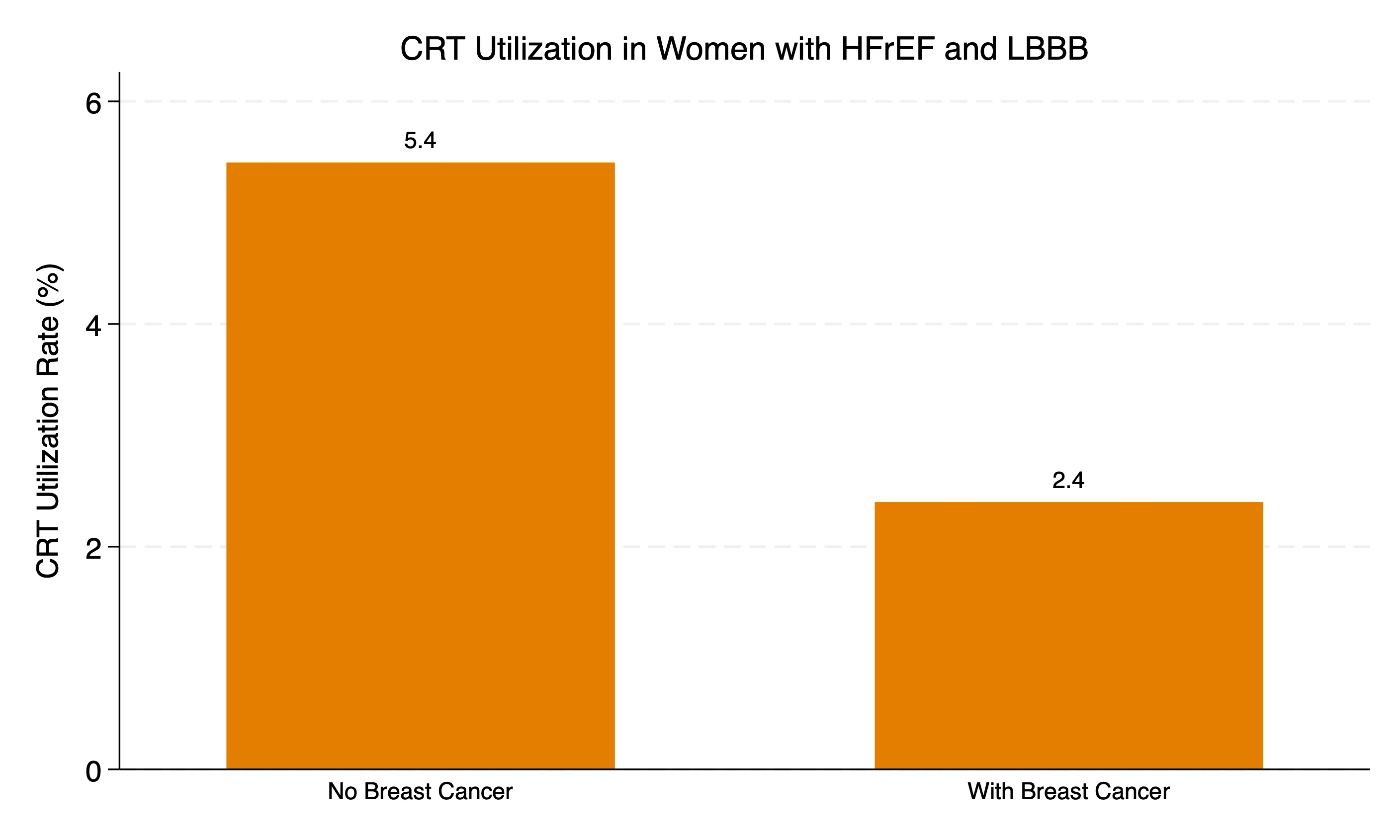
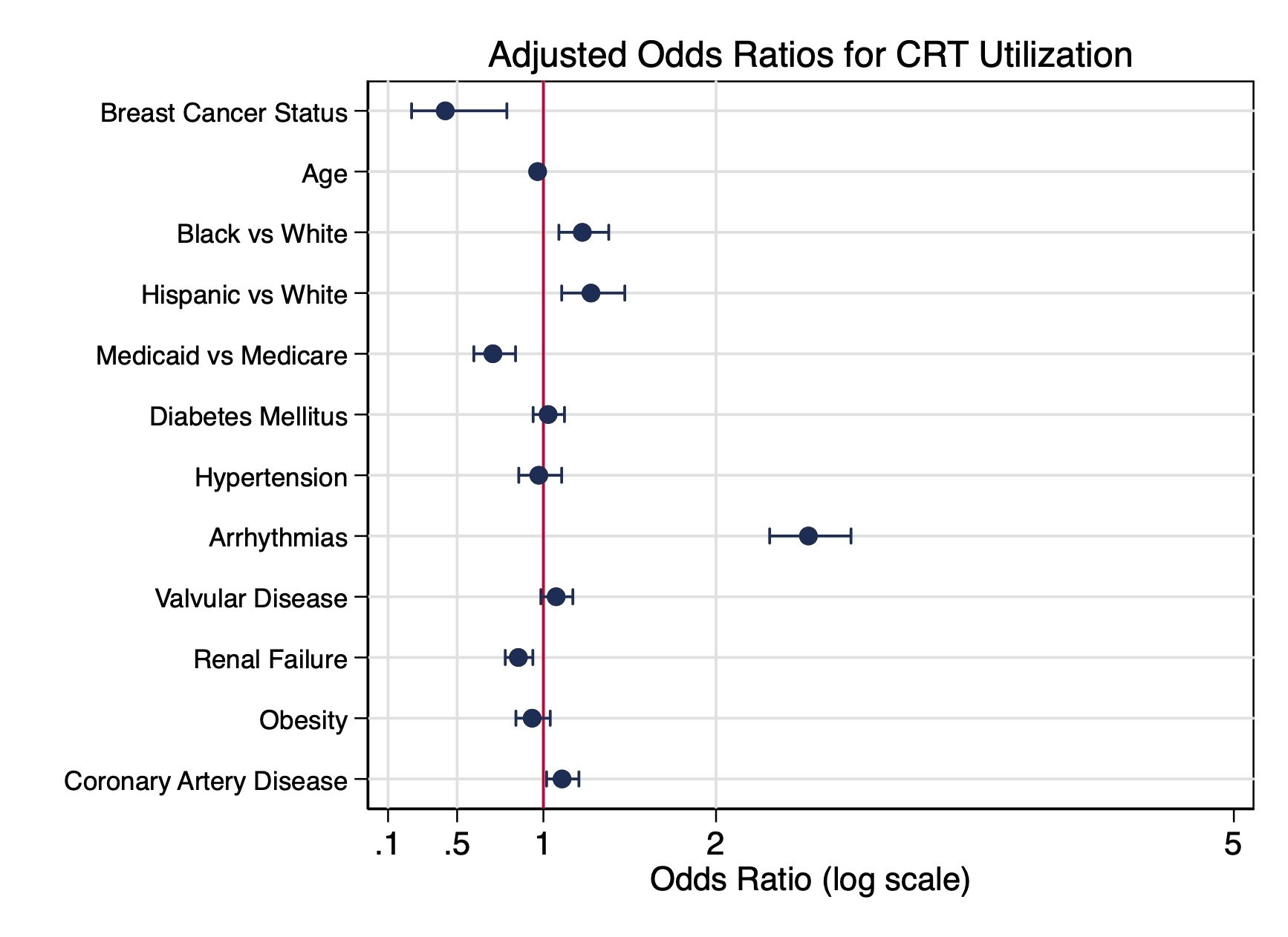
CRT utilization was significantly lower in the breast cancer group (2.4% vs. 5.45%, p <0.01). After adjusting for age, race, comorbidities, and payer type, breast cancer remained independently associated with reduced CRT use (aOR 0.43, 95% CI 0.24–0.79).
Conclusion:
Women with breast cancer and HFrEF with LBBB are significantly less likely to receive CRT despite potential benefits. Given the high survivorship rates, these findings underscore the need to address disparities and optimize long-term cardiac care.
Cardiac resynchronization therapy (CRT) has been demonstrated to reduce both mortality and morbidity in patients with LBBB. Despite this, CRT remains underutilized in certain populations, particularly among women. Breast cancer generally has a high five-year survival rate of 91% and is commonly treated with cardiotoxic chemotherapy, which increases the risk of HFrEF. Given the risk and potential benefits of CRT, its application in breast cancer patients may be valuable. However, clinical bias or concerns regarding cancer status may contribute to its underuse. This study aims to evaluate disparities in CRT utilization among female patients with breast cancer.
Research Question:
To investigate the disparity in CRT utilization among female patients with breast cancer and HFrEF with LBBB compared to those without.
Methods:
We conducted a cross-sectional study using the National Inpatient Sample (2016-2022) to identify adult female hospitalizations with a diagnosis of HFrEF and LBBB. The history of breast cancer was determined using ICD-10-CM codes. Survey-weighted analyses were used to compare baseline characteristics and outcomes, including CRT use, in-hospital mortality, length of stay, and comorbidities. Logistic regression was performed to adjust for potential confounders.
Results:
A total of 47,437 adult women with HFrEF and LBBB were included in the analysis. Of these, 2,295 (1.0%) had breast cancer. Compared to non-cancer patients, those with breast cancer were younger (73.4 vs. 74.9 years, p < 0.01), had a lower prevalence of renal failure (27.7% vs. 36.6%, p < 0.01), valvular disease (28.3% vs. 35.3%, p <0.01), and anemia (10.5% vs. 7.4%, p = 0.01). No significant differences were observed in diabetes or obesity between the two groups. In-hospital mortality (5.2% vs. 4.3%, p = 0.33), length of stay (5.9 vs. 5.6 days), and arrhythmia burden (50.5% vs. 55.8%) were comparable between groups.
CRT utilization was significantly lower in the breast cancer group (2.4% vs. 5.45%, p <0.01). After adjusting for age, race, comorbidities, and payer type, breast cancer remained independently associated with reduced CRT use (aOR 0.43, 95% CI 0.24–0.79).
Conclusion:
Women with breast cancer and HFrEF with LBBB are significantly less likely to receive CRT despite potential benefits. Given the high survivorship rates, these findings underscore the need to address disparities and optimize long-term cardiac care.
More abstracts on this topic:
Ambulatory Inotropic Support in Patients with Stage D Heart Failure Does Not Increase ICD Therapies
Sunthankar Kathryn, Pfaff Jamie, Farber-eger Eric, Richardson Travis, Wells Quinn, Ooi Henry, Skelton Melanie, Stevenson Lynne, Pedrotty Dawn
Left Atrial Reservoir Phase Duration and Long-Term Survival After Cardiac Resynchronization TherapyHammersboen Lars-egil, Sletten Ole Jakob, Penicka Martin, Donal Erwan, Voigt Jens-uwe, Smiseth Otto, Stugaard Marie, Aalen John, Puvrez Alexis, Larsen Camilla, Remme Espen, Kongsgaard Erik, Duchenne Jurgen, Galli Elena, Khan Faraz