Final ID: MP483
Shifting Trends in Type 1 and Type 2 Myocardial Infarction Diagnoses and Mortality: A National Inpatient Sample Analysis
Abstract Body (Do not enter title and authors here): Background: The 2018 Fourth Universal Definition of Myocardial Infarction reclassified it into five subtypes, including type 1 myocardial infarction (T1MI), due to acute atherothrombotic coronary occlusion, and type 2 myocardial infarction (T2MI), resulting from myocardial oxygen supply-demand mismatch. In 2017, a specific ICD-10-CM code for T2MI was introduced, increasing its clinical recognition to medical providers. However, national trends in diagnosis and outcomes remain limited. This study evaluates temporal patterns in T1MI and T2MI diagnoses and associated in-hospital outcomes using a nationally representative sample.
Research Questions: We hypothesized that the clinical recognition of T2MI has increased over time.
Methods: We conducted a serial cross-sectional analysis of the National Inpatient Sample from 2017 to 2022. Adult hospitalizations with a primary or secondary diagnosis of T1MI or T2MI were identified using ICD-10-CM codes. Outcomes included trends in hospitalization volume, in-hospital mortality, length of stay, and percutaneous coronary intervention (PCI) rates. Multivariable survey-weighted logistic and linear regression models adjusted for demographics and comorbidities using Elixhauser categories.
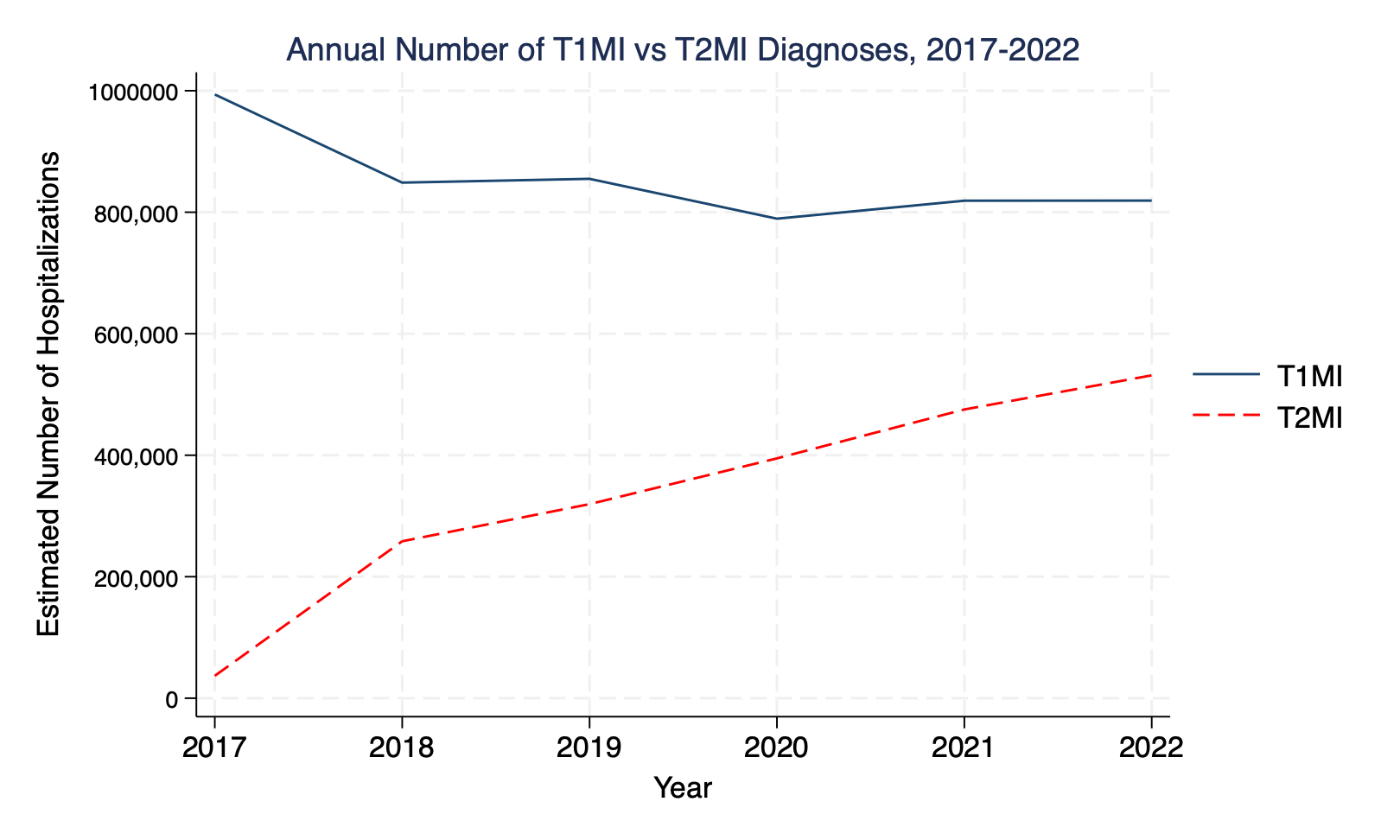
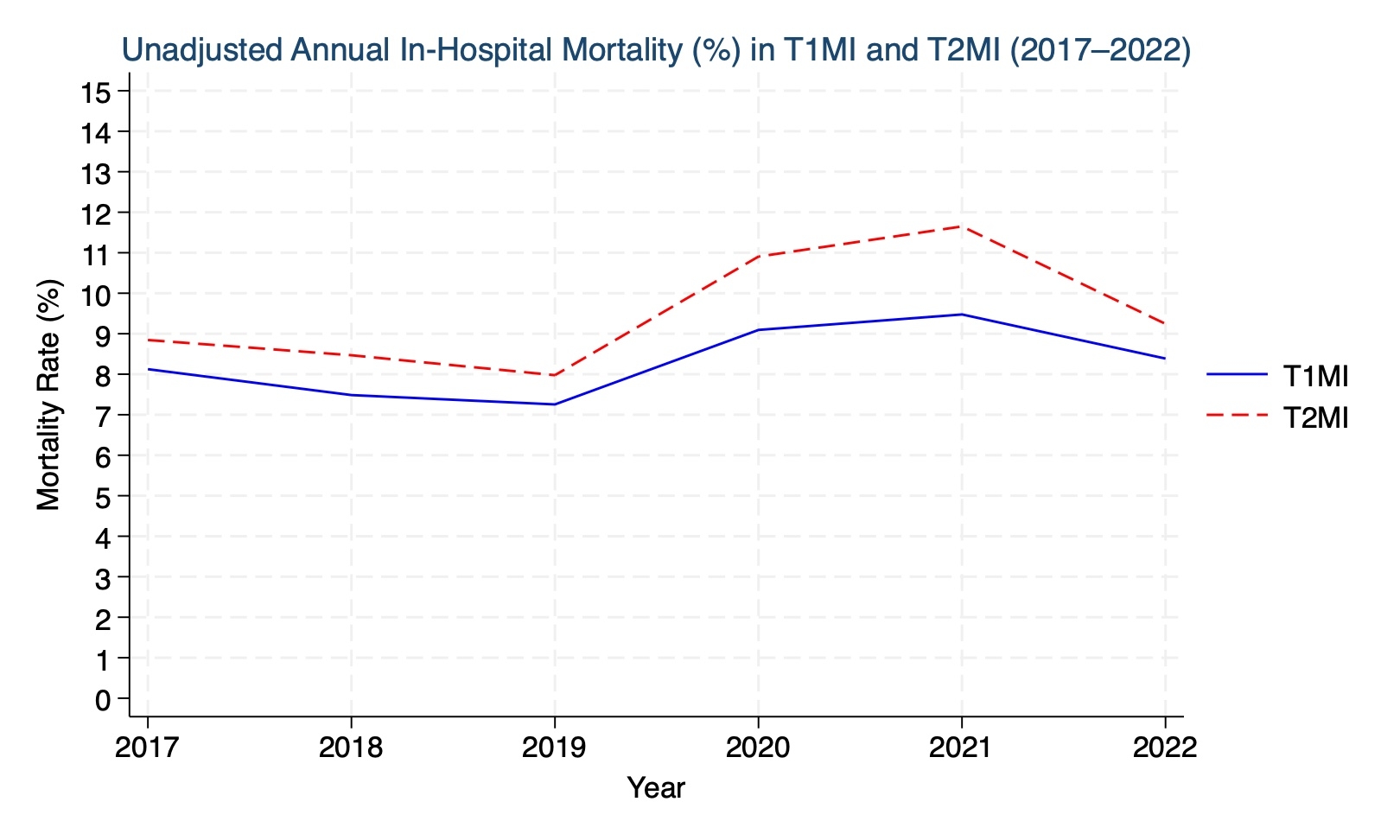
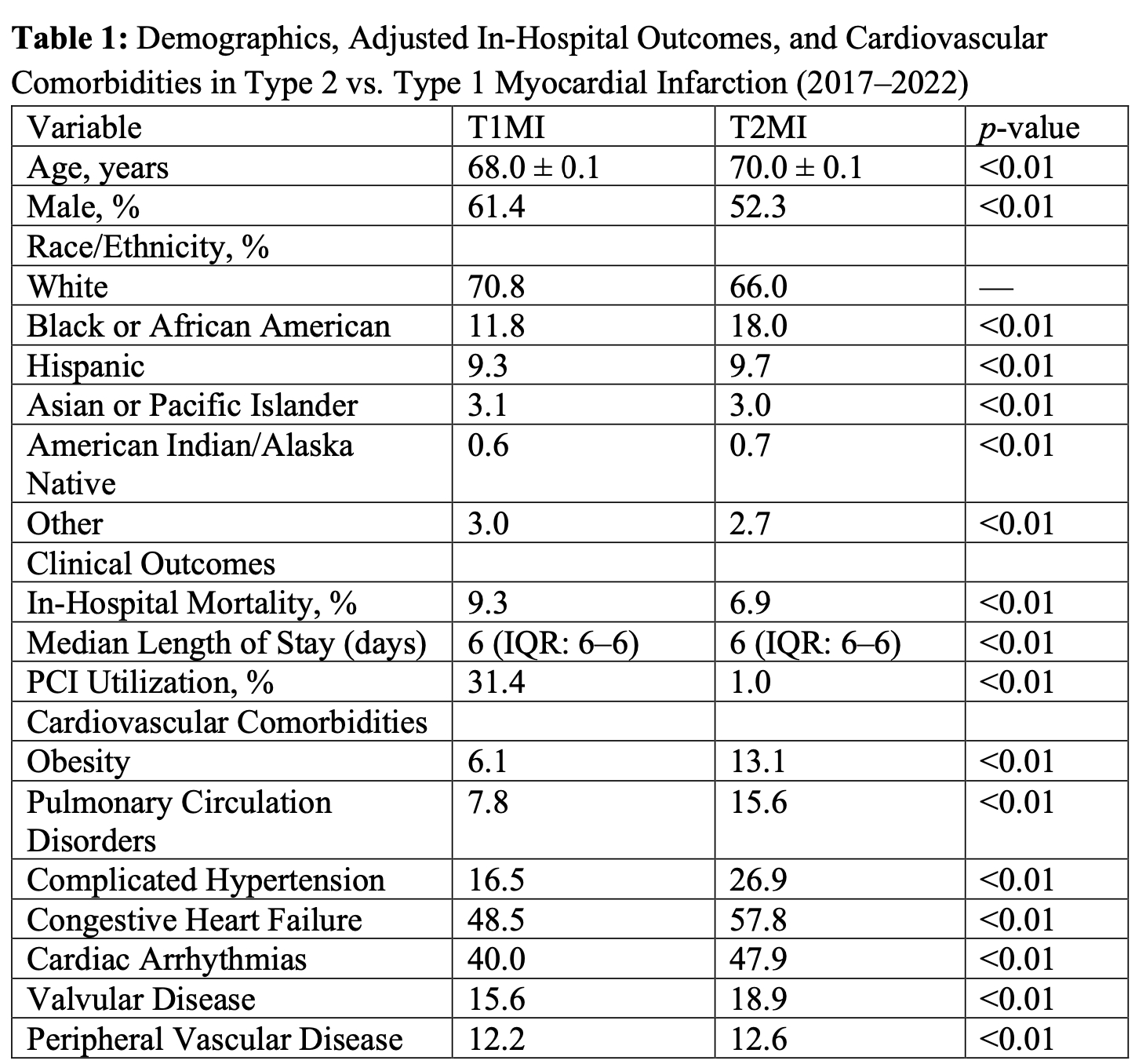
Results: Among 7,119,208 MI hospitalizations, 5,102,779 (71.7%) were T1MI and 2,016,429 (28.3%) were T2MI. T2MI diagnoses increased 14-fold from 36,915 in 2017 to 531,445 in 2022, rising from 3.6% to 39.5% of MI cases. In contrast, T1MI diagnoses declined by 18.5%, with its proportion dropping from 96.4% in 2017 to 60.5% in 2022. T2MI patients were older, more often female, and had a higher cardiovascular comorbidity burden as shown in Table 1. The most strongly associated cardiovascular comorbidities with T2MI were obesity (aOR 2.58), pulmonary circulation disorders (aOR 2.18), complicated hypertension (aOR 1.65), congestive heart failure (aOR 1.45), and cardiac arrhythmias (aOR 1.39). Adjusted in-hospital mortality was lower in T2MI (6.9%) compared to T1MI (9.3%), while median LOS was similar (6 days in both). PCI use remained substantially lower in T2MI (1.0% vs. 31.4%).
Conclusions: T2MI diagnoses have risen after the adoption of a new definition of myocardial infarction, while T1MI diagnoses have declined. Despite higher crude mortality, adjusted outcomes suggest lower mortality in T2MI. These findings underscore the need for dedicated management pathways and cardiovascular risk profiling for this growing population.
Research Questions: We hypothesized that the clinical recognition of T2MI has increased over time.
Methods: We conducted a serial cross-sectional analysis of the National Inpatient Sample from 2017 to 2022. Adult hospitalizations with a primary or secondary diagnosis of T1MI or T2MI were identified using ICD-10-CM codes. Outcomes included trends in hospitalization volume, in-hospital mortality, length of stay, and percutaneous coronary intervention (PCI) rates. Multivariable survey-weighted logistic and linear regression models adjusted for demographics and comorbidities using Elixhauser categories.
Results: Among 7,119,208 MI hospitalizations, 5,102,779 (71.7%) were T1MI and 2,016,429 (28.3%) were T2MI. T2MI diagnoses increased 14-fold from 36,915 in 2017 to 531,445 in 2022, rising from 3.6% to 39.5% of MI cases. In contrast, T1MI diagnoses declined by 18.5%, with its proportion dropping from 96.4% in 2017 to 60.5% in 2022. T2MI patients were older, more often female, and had a higher cardiovascular comorbidity burden as shown in Table 1. The most strongly associated cardiovascular comorbidities with T2MI were obesity (aOR 2.58), pulmonary circulation disorders (aOR 2.18), complicated hypertension (aOR 1.65), congestive heart failure (aOR 1.45), and cardiac arrhythmias (aOR 1.39). Adjusted in-hospital mortality was lower in T2MI (6.9%) compared to T1MI (9.3%), while median LOS was similar (6 days in both). PCI use remained substantially lower in T2MI (1.0% vs. 31.4%).
Conclusions: T2MI diagnoses have risen after the adoption of a new definition of myocardial infarction, while T1MI diagnoses have declined. Despite higher crude mortality, adjusted outcomes suggest lower mortality in T2MI. These findings underscore the need for dedicated management pathways and cardiovascular risk profiling for this growing population.
More abstracts on this topic:
A Novel Cardioprotective Mechanism in Myocardial Reperfusion Injury: Dual Neutrophil Modulation and ROS/HOCl Scavenging by an Atypical Chemokine
Zwissler Leon, Bernhagen Juergen, Cabrera-fuentes Hector Alejandro, Hernandez Resendiz Sauri, Yap En Ping, Schindler Lisa, Zhang Zhishen, Dickerhof Nina, Hampton Mark, Liehn Elisa, Hausenloy Derek
A Case of Immune Checkpoint Inhibitor-Induced Myocarditis with Myositis and/or Myasthenia Gravis Overlap Syndrome with New Right Bundle Branch Block and Negative Cardiac MRIDasari Srikiran