Final ID: MP1622
Systemic Inflammation Response Index Predicts 30-Day Mortality in Vietnamese Acute Heart Failure Patients
Abstract Body (Do not enter title and authors here): Introduction
Inflammation plays a important role in determining the prognosis of heart failure. Recent studies have demonstrated that both established and novel inflammatory biomarkers—such as the neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR), platelet-to-lymphocyte ratio (PLR), Systemic Immune-Inflammation Index (SII), and, in particular, the Systemic Inflammation Response Index (SIRI)—serve as important predictors of mortality in heart failure patients. Nonetheless, data from developing countries like Vietnam remain limited.
Hypothesis
Inflammatory markers are associated with 30-day all-cause mortality in patients hospitalized with acute heart failure (AHF).
Methods
We performed a prospective cohort study at Can Tho Central General Hospital—a tertiary care center in Vietnam—from May 2024 through April 2025. Consecutive adults (≥18 years) admitted with acute heart failure (NT-proBNP >300 pg/mL) who provided informed consent were enrolled, while those with active infection, immunosuppressant use within the prior three months, chronic liver disease, or active malignancy were excluded. Survivors were followed for 30 days after discharge, with all-cause mortality as the primary endpoint. Relative risks were derived from a modified Poisson log-linear regression using a robust (sandwich) variance estimator, adjusting for baseline demographics and comorbidities.
Results
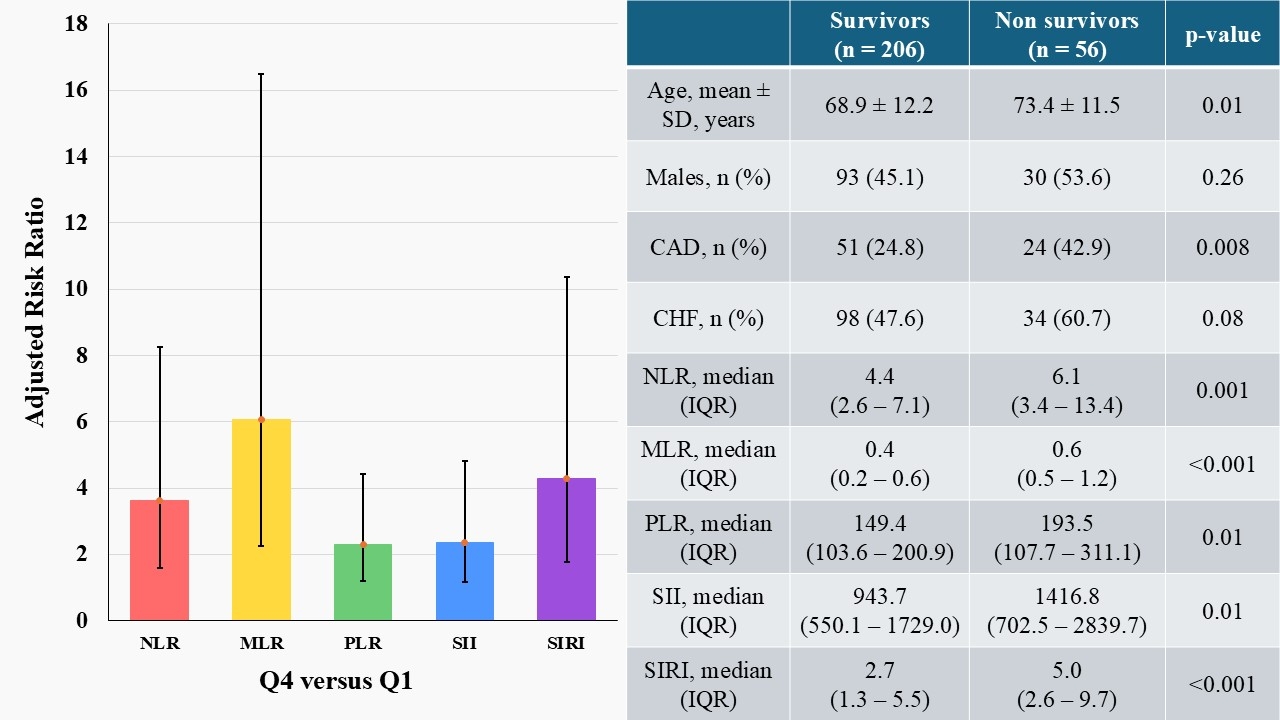
Among 411 AHF patients (mean age 69.6 ± 12.6 years; 47.4 % men), 262 (63.7 %) completed 30-day follow-up, during which 56 deaths occurred (all-cause mortality 21.4 %). Non-survivors were older, carried a greater comorbidity burden, and exhibited higher median levels of NLR, MLR, PLR, SII, and SIRI than survivors. In multivariable Poisson models adjusted for age, sex, coronary artery disease, prior heart failure, hypertension, and diabetes, individuals in the highest biomarker quartile had markedly increased 30-day mortality risk compared with those in the lowest quartile: NLR (RR 3.6; 95 % CI 1.6–8.3), MLR (RR 6.1; 95 % CI 2.2–16.5), PLR (RR 2.3; 95 % CI 1.2–4.4), SII (RR 2.4; 95 % CI 1.2–4.8), and SIRI (RR 4.3; 95 % CI 1.8–10.4).
Conclusion
Inflammatory markers independently predict 30-day mortality in Vietnamese AHF patients; adding them to risk models may enhance short-term prognosis, while its longer-term predictive value warrants further investigation.
Inflammation plays a important role in determining the prognosis of heart failure. Recent studies have demonstrated that both established and novel inflammatory biomarkers—such as the neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR), platelet-to-lymphocyte ratio (PLR), Systemic Immune-Inflammation Index (SII), and, in particular, the Systemic Inflammation Response Index (SIRI)—serve as important predictors of mortality in heart failure patients. Nonetheless, data from developing countries like Vietnam remain limited.
Hypothesis
Inflammatory markers are associated with 30-day all-cause mortality in patients hospitalized with acute heart failure (AHF).
Methods
We performed a prospective cohort study at Can Tho Central General Hospital—a tertiary care center in Vietnam—from May 2024 through April 2025. Consecutive adults (≥18 years) admitted with acute heart failure (NT-proBNP >300 pg/mL) who provided informed consent were enrolled, while those with active infection, immunosuppressant use within the prior three months, chronic liver disease, or active malignancy were excluded. Survivors were followed for 30 days after discharge, with all-cause mortality as the primary endpoint. Relative risks were derived from a modified Poisson log-linear regression using a robust (sandwich) variance estimator, adjusting for baseline demographics and comorbidities.
Results
Among 411 AHF patients (mean age 69.6 ± 12.6 years; 47.4 % men), 262 (63.7 %) completed 30-day follow-up, during which 56 deaths occurred (all-cause mortality 21.4 %). Non-survivors were older, carried a greater comorbidity burden, and exhibited higher median levels of NLR, MLR, PLR, SII, and SIRI than survivors. In multivariable Poisson models adjusted for age, sex, coronary artery disease, prior heart failure, hypertension, and diabetes, individuals in the highest biomarker quartile had markedly increased 30-day mortality risk compared with those in the lowest quartile: NLR (RR 3.6; 95 % CI 1.6–8.3), MLR (RR 6.1; 95 % CI 2.2–16.5), PLR (RR 2.3; 95 % CI 1.2–4.4), SII (RR 2.4; 95 % CI 1.2–4.8), and SIRI (RR 4.3; 95 % CI 1.8–10.4).
Conclusion
Inflammatory markers independently predict 30-day mortality in Vietnamese AHF patients; adding them to risk models may enhance short-term prognosis, while its longer-term predictive value warrants further investigation.
More abstracts on this topic:
A Remote Patient Care Heart Failure Program Drives Improved Clinical Outcomes and Reduced Healthcare Cost and Utilization
Feldman David, Reynolds Spencer, Curnow Randall, Cunningham Eve, Feldman Theodore, Fudim Marat
A Meta-Analysis of Prospective Studies Comparing Short and Longterm Outcomes of Trans-Catheter Aortic Valve Replacement in Patient with and without Cancer:Khan Muhammad Aslam, Haider Adnan, Haider Taimoor, Bhattarai Shraddha, Khan Bilal, Lamichhane Bikal, Shafique Nouman, Rahman Hammad, Aafreen Asna, Muhammad Anza, Bhatia Hitesh, Khan Abid Nawaz Khan, Akbar Usman, Khan Alamzaib