Final ID: MP1537
Social determinants of health screen rates, positive screens, and outcomes for cardiovascular patients within a large health network in Oregon
Abstract Body (Do not enter title and authors here): Background: Social determinants of health (SDOH) are tied to cardiovascular disease (CVD) prevalence, disease progression, and outcomes. New federal and Oregon requirements mandate SDOH screening in inpatient and primary care settings.
Objective: Examine rates and predictors of SDOH screening, positive screens, and clinical outcomes for CVD patients.
Methods: Retrospective cohort study of all CVD patients who received care in the 7 hospitals and 63 outpatient cardiology clinics in the Providence Oregon network between 10/01/2023 – 4/24/25. In-hospital admissions with a CVD primary diagnosis, outpatient cardiology encounters, and outpatient cardiology referrals were included. SDOH screening included the following six domains: food, housing, transportation, utilities, financial strain, and intimate partner violence. SDOH screenings, patient characteristics, comorbidities, and outcomes were obtained from the electronic medical record. Rural-urban commuting area (RUCA) and the Center for Disease Control & Prevention social vulnerability index (SVI) were linked to patient home address. The primary outcome was a positive screen in ≥1 SDOH domain. Secondary outcomes were new CVD or related comorbidities after the positive screen and 1-year mortality. Logistic regression models accounting for age, sex, race, ethnicity, insurance, RUCA, and SVI were run.
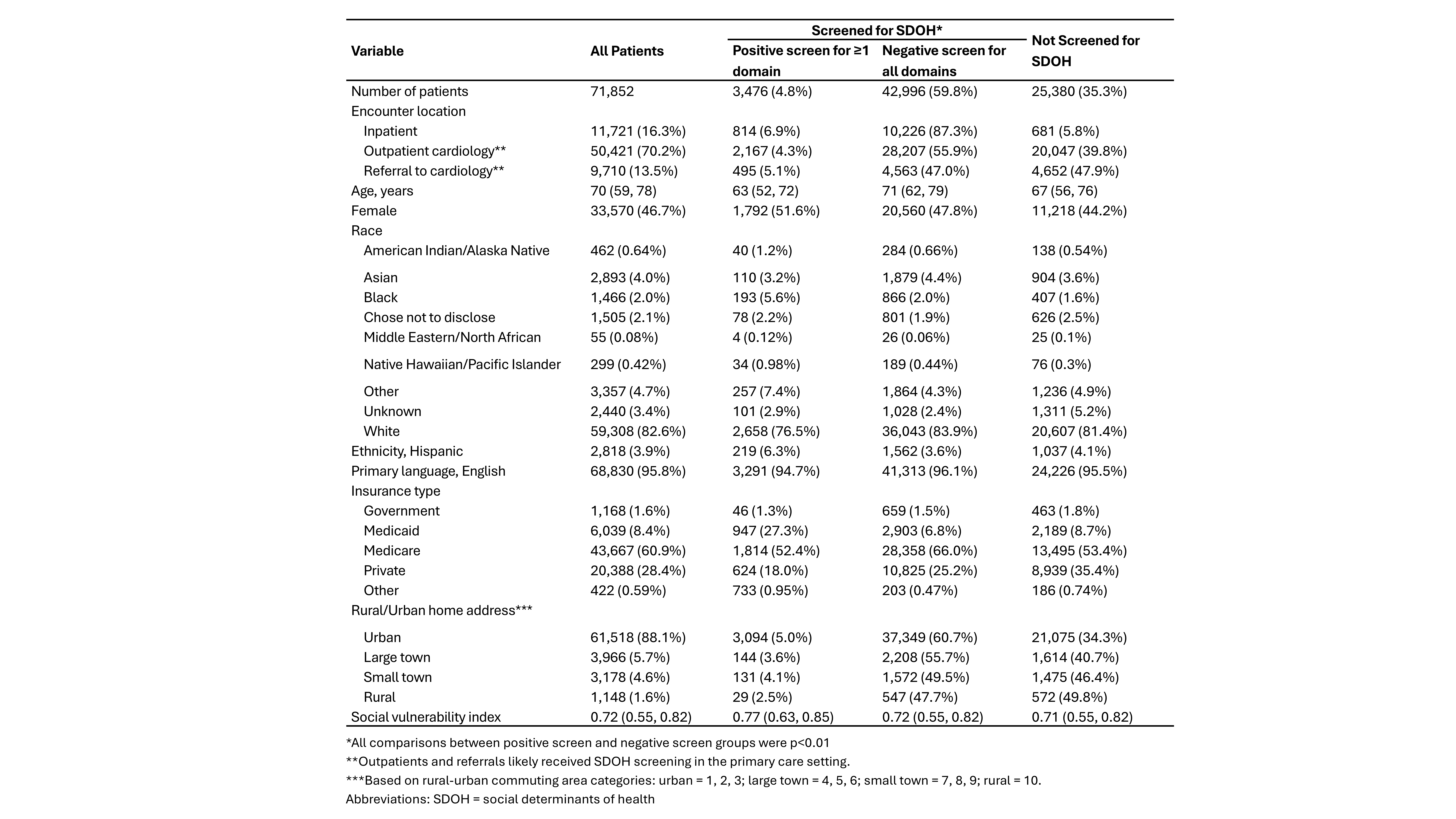
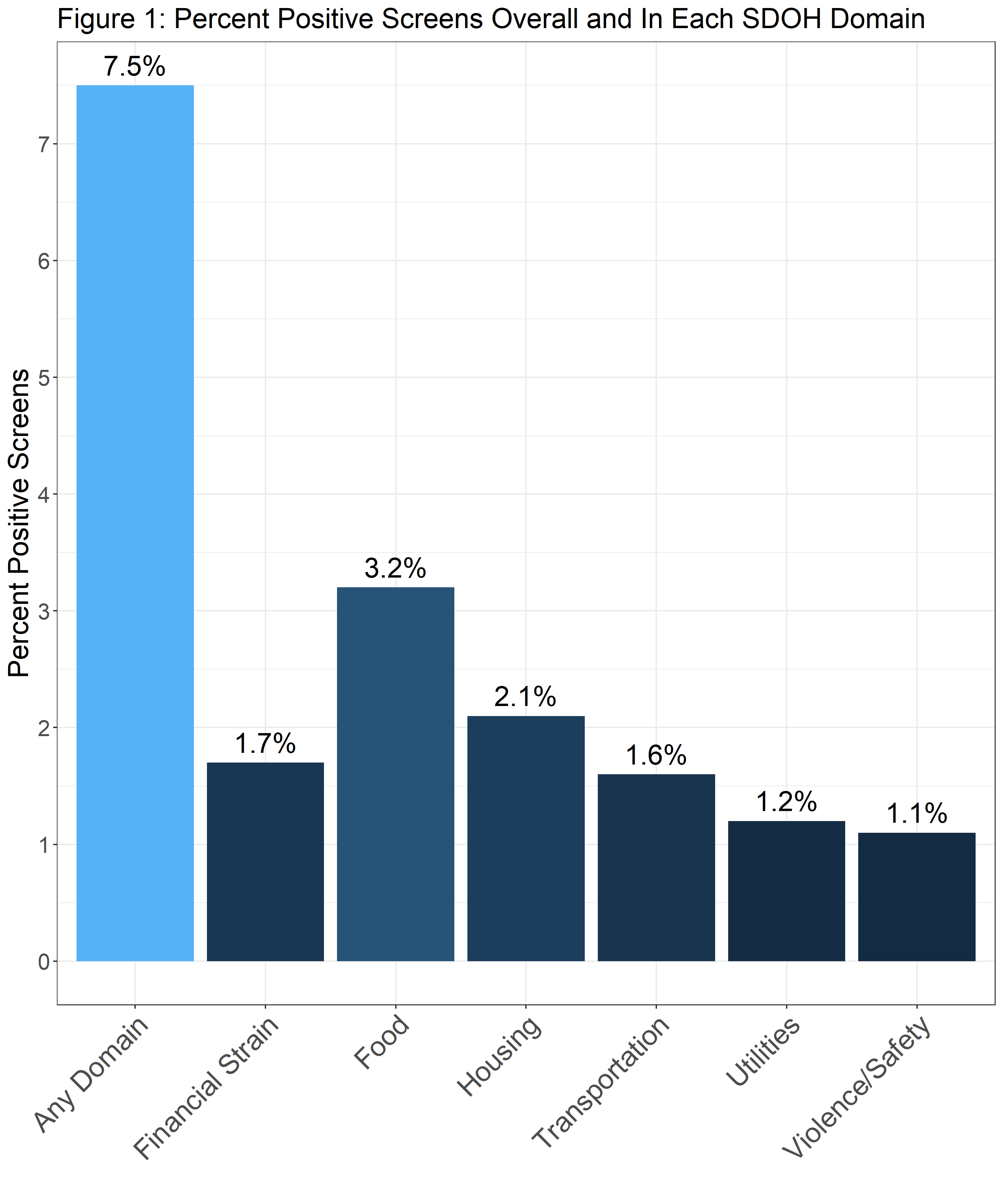
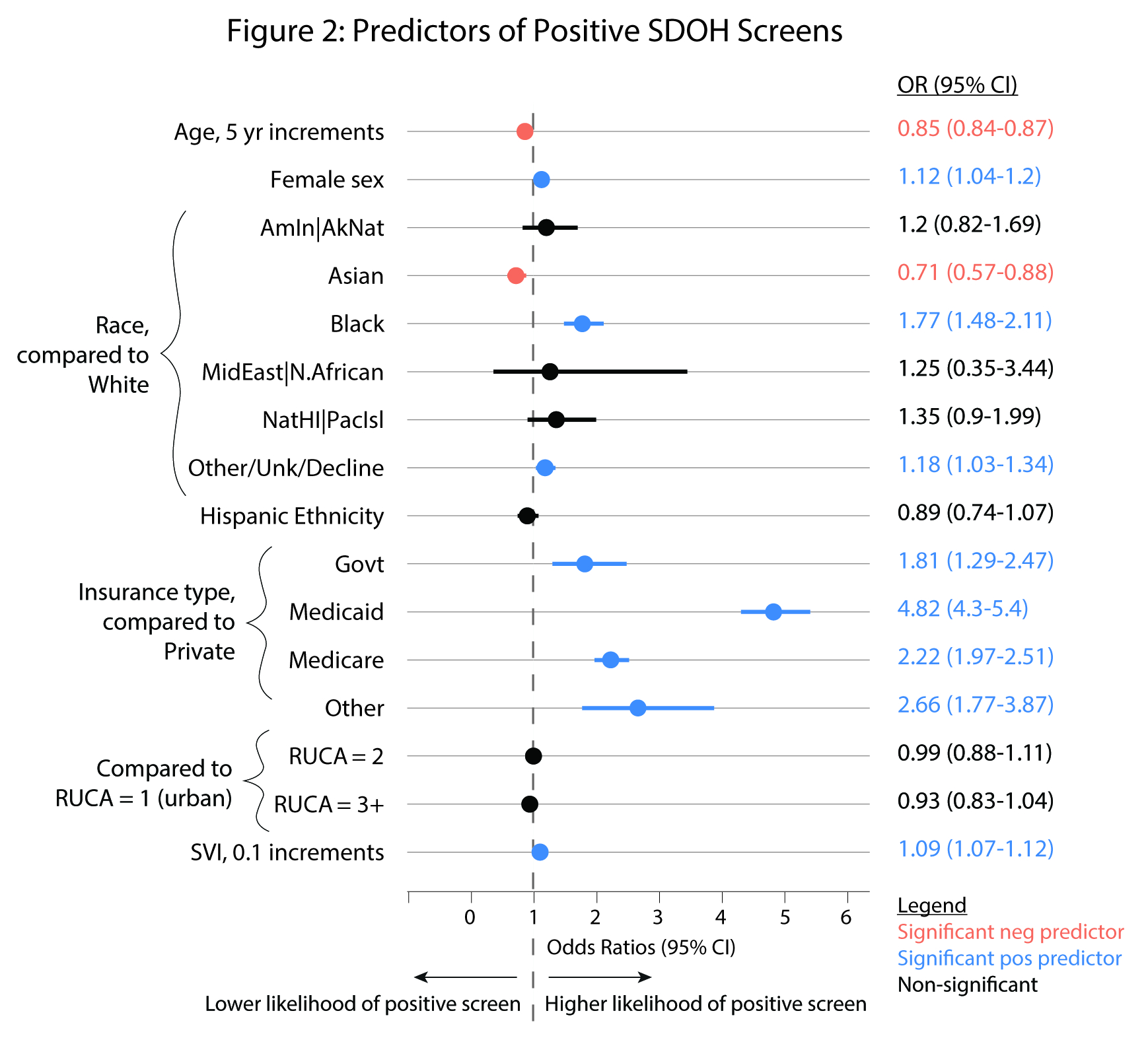
Results: There were 71,852 CVD patients included, the majority of whom were seen at an outpatient cardiology clinic (70%) (Table 1). Across all settings, 65% of patients were screened for SDOH and 4.8% had a positive screen. Screening rate and positive screens were highest in the inpatient setting (94% and 6.9%, respectively). Patients with positive screens were significantly younger, more often Black, American Indian, Native Hawaiian, or of other or unknown races, Hispanic ethnicity, and had higher rates of Medicaid insurance (27%). Of patients screened, 7.5% screened positive, with the highest rates in the food and housing domains (Figure 1). Predictors of positive screens are shown in Figure 2. Positive screens were not associated with greater odds of new CVD or 1-year mortality.
Conclusions: Following new regulatory requirements, there is a high rate of screening for SDOH within our health system. Positive screens were more common in populations with known health disparities, yet preliminary results suggest positive screens may not be associated with short term negative cardiovascular outcomes.
Objective: Examine rates and predictors of SDOH screening, positive screens, and clinical outcomes for CVD patients.
Methods: Retrospective cohort study of all CVD patients who received care in the 7 hospitals and 63 outpatient cardiology clinics in the Providence Oregon network between 10/01/2023 – 4/24/25. In-hospital admissions with a CVD primary diagnosis, outpatient cardiology encounters, and outpatient cardiology referrals were included. SDOH screening included the following six domains: food, housing, transportation, utilities, financial strain, and intimate partner violence. SDOH screenings, patient characteristics, comorbidities, and outcomes were obtained from the electronic medical record. Rural-urban commuting area (RUCA) and the Center for Disease Control & Prevention social vulnerability index (SVI) were linked to patient home address. The primary outcome was a positive screen in ≥1 SDOH domain. Secondary outcomes were new CVD or related comorbidities after the positive screen and 1-year mortality. Logistic regression models accounting for age, sex, race, ethnicity, insurance, RUCA, and SVI were run.
Results: There were 71,852 CVD patients included, the majority of whom were seen at an outpatient cardiology clinic (70%) (Table 1). Across all settings, 65% of patients were screened for SDOH and 4.8% had a positive screen. Screening rate and positive screens were highest in the inpatient setting (94% and 6.9%, respectively). Patients with positive screens were significantly younger, more often Black, American Indian, Native Hawaiian, or of other or unknown races, Hispanic ethnicity, and had higher rates of Medicaid insurance (27%). Of patients screened, 7.5% screened positive, with the highest rates in the food and housing domains (Figure 1). Predictors of positive screens are shown in Figure 2. Positive screens were not associated with greater odds of new CVD or 1-year mortality.
Conclusions: Following new regulatory requirements, there is a high rate of screening for SDOH within our health system. Positive screens were more common in populations with known health disparities, yet preliminary results suggest positive screens may not be associated with short term negative cardiovascular outcomes.
More abstracts on this topic:
An Evaluation of Bystander CPR by Race, Accounting for Social Drivers of Health
Lane Nina, Crowe Remle, Salcido David
A Quarter Century of Cardiovascular Strain: Mortality Trends in Hypertension and Hypertensive Heart Disease Among U.S. Adults Aged 55+Ali Muhammad Faizan, Khan Muhammad, Sharif Aleena, Hossain Mohammad, Ahmad Husnain, Eltawansy Sherif, Faizan Muhammad, Ahmed Ashraf, Abdul Malik Mohammad Hamza Bin, Pahwani Ritesh, Patel Rahul, Mehdi Hassan