Final ID: MP181
Low rates of cardiotoxicity during HER2-directed antibody therapy for breast cancer across a large, Western US hospital system
Abstract Body (Do not enter title and authors here): Background: HER2-directed antibodies (anti-HER2) are associated with cardiotoxicity and guidelines recommend routine cardiac monitoring. Recent studies suggest a wide range of cardiotoxicity incidence between 4-30%. Our goal was to characterize anti-HER2-associated cardiotoxicity incidence in a real-world clinical setting and evaluate for predictors of cardiotoxicity.
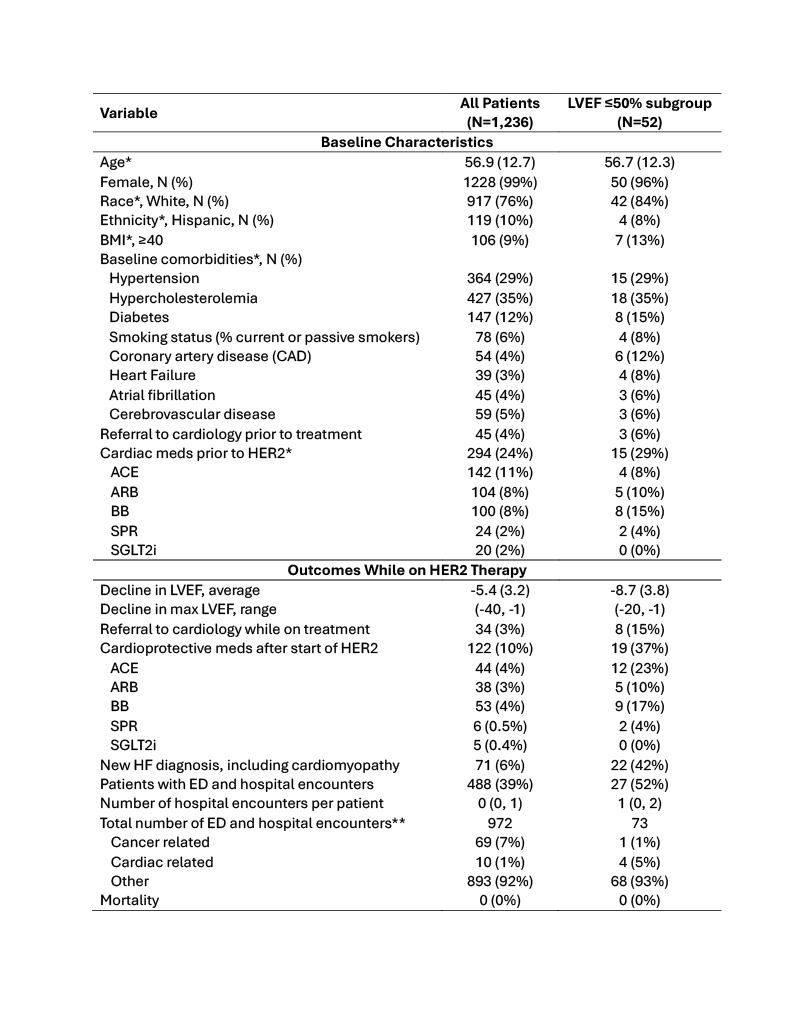
Methods: We performed a retrospective cohort study of early stage (I-III) breast cancer (BC) patients who received anti-HER2 between 1/1/2016-3/20/2024 in the 7-state Providence St. Joseph Health network. Patients with baseline left ventricle ejection fraction (LVEF) assessment and at least one on-treatment assessment were included. Demographics, medications, clinical and LVEF data, and outcomes were obtained from the electronic medical record. The primary outcome was development of LVEF ≤50% during anti-HER2. Secondary outcomes included new heart failure (HF) diagnosis, hospitalization, and mortality. Logistic regression models accounting for demographics, baseline comorbidities, and cardiac medications prior to HER2 were run.
Results: The study included 1,236 patients (mean age 57, 99% female) (Table). Prior to anti-HER2, 24% of patients were on cardiac medications and 4% had referrals to cardiology, indicating baseline cardiac disease. Fifty-two (4%) patients developed LVEF ≤50% during anti-HER2. In the LVEF ≤50% group, average decline in LVEF during therapy was -8.7%[LM1] . For patients who developed LVEF ≤50%, 15% were referred to cardiology, 37% were started on new cardiac medications, and 42% had a new diagnosis of HF. Compared to the overall group, a higher number of patients developing LVEF ≤50% were hospitalized (52% vs 39%). No patients died while receiving anti-HER2 or during the follow up period. Baseline coronary artery disease (CAD) was the only predictor of LVEF ≤50% during therapy (aOR=3.11 [1.04, 9.31]).
Conclusions: In a real-world clinical setting, anti-HER2-associated LVEF declines were uncommon but were associated with increased hospitalizations and formal HF diagnoses. LVEF declines were predominantly in patients with baseline CAD, highlighting the importance of close LVEF monitoring in this population. Patients without risk factors may be at reduced risk of cardiotoxicity and hence de-escalating imaging surveillance may be considered with future studies.
Methods: We performed a retrospective cohort study of early stage (I-III) breast cancer (BC) patients who received anti-HER2 between 1/1/2016-3/20/2024 in the 7-state Providence St. Joseph Health network. Patients with baseline left ventricle ejection fraction (LVEF) assessment and at least one on-treatment assessment were included. Demographics, medications, clinical and LVEF data, and outcomes were obtained from the electronic medical record. The primary outcome was development of LVEF ≤50% during anti-HER2. Secondary outcomes included new heart failure (HF) diagnosis, hospitalization, and mortality. Logistic regression models accounting for demographics, baseline comorbidities, and cardiac medications prior to HER2 were run.
Results: The study included 1,236 patients (mean age 57, 99% female) (Table). Prior to anti-HER2, 24% of patients were on cardiac medications and 4% had referrals to cardiology, indicating baseline cardiac disease. Fifty-two (4%) patients developed LVEF ≤50% during anti-HER2. In the LVEF ≤50% group, average decline in LVEF during therapy was -8.7%[LM1] . For patients who developed LVEF ≤50%, 15% were referred to cardiology, 37% were started on new cardiac medications, and 42% had a new diagnosis of HF. Compared to the overall group, a higher number of patients developing LVEF ≤50% were hospitalized (52% vs 39%). No patients died while receiving anti-HER2 or during the follow up period. Baseline coronary artery disease (CAD) was the only predictor of LVEF ≤50% during therapy (aOR=3.11 [1.04, 9.31]).
Conclusions: In a real-world clinical setting, anti-HER2-associated LVEF declines were uncommon but were associated with increased hospitalizations and formal HF diagnoses. LVEF declines were predominantly in patients with baseline CAD, highlighting the importance of close LVEF monitoring in this population. Patients without risk factors may be at reduced risk of cardiotoxicity and hence de-escalating imaging surveillance may be considered with future studies.
More abstracts on this topic:
A Curious Complete Heart Block with Carfilzomib
Shah Mohammed, Rahman Naveed, Al-mohamad Talal, Batra Sejal, Vyas Apurva
A Comparison Between Global Longitudinal Strain (GLS) Derived with CMR Feature-Tracking (CMR-FT) and 2D Speckle-Tracking Echocardiography (2D-STE) to Monitor Cancer Therapy-Related Cardiac Dysfunction (CTRCD)Kar Julia, Cohen Michael, Revere Cherie, Mcquiston Samuel, Malozzi Christopher