Final ID: MP1641
The Obesity Paradox Still Exists in Heart Failure: A Dose-Response Meta-Analysis of Body Mass Index and Mortality Across Diverse Subgroups
Abstract Body (Do not enter title and authors here): Background: Despite obesity being a major cardiovascular risk factor, studies in heart failure populations have reported an inverse association between body mass index and mortality—a phenomenon termed the "obesity paradox." However, the consistency and shape of this relationship across different HF phenotypes and clinical subgroups remain unclear. This meta-analysis aimed to quantify the dose-response relationship between BMI and mortality in HF patients and assess potential variations across subgroups.
Hypothesis: Higher BMI is associated with reduced mortality in patients with heart failure, and that this relationship varies across clinical subgroups and U-shaped relationship.
Methods: We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. A search strategy was developed, and studies were extracted from Cochrane and PubMed databases through December 2023. The main outcomes were all-cause mortality, cardiovascular deaths, and heart failure hospitalizations. Data were summarized as hazard ratios with 95% confidence intervals, and a spline model was used to assess non-linear relationships, with 21.7 kg/m2 as the reference point in the dose-response curve. PROSPERO: CRD42023455124
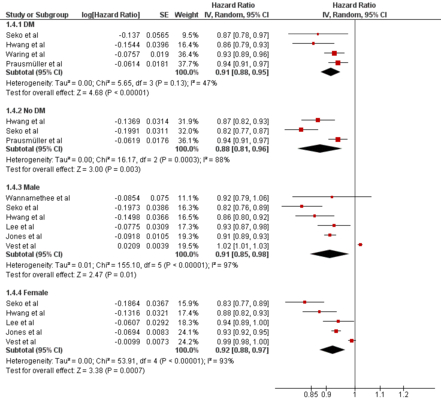
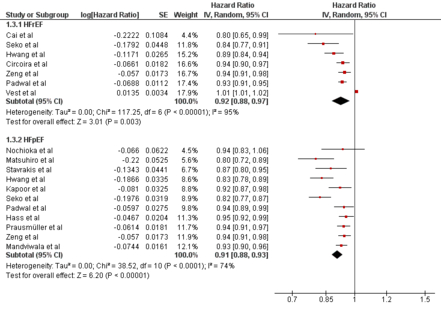
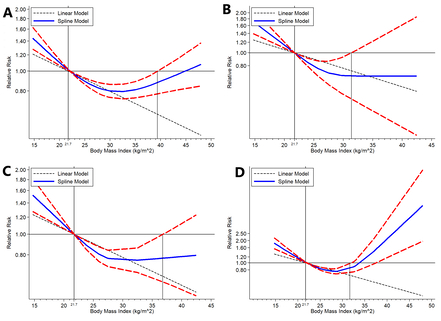
Results: Thirty-three studies (457,124 person-years) showed that each 5 kg/m2 increase in BMI was significantly associated with a 6% reduction in all-cause mortality (HR 0.94; 95% CI 0.92–0.96). Significant reductions were observed in acute decompensated heart failure (7%), HFpEF (9%), HFrEF (8%), diabetes (9%), males (9%), and females (8%). Cardiovascular mortality declined by 5% per 5 kg/m2 increase. Non-linear analysis revealed a significant U-shaped relationship, with lowest all-cause mortality between BMI 21.7 and 39 kg/m2. Subgroup analysis showed significant non-linear all-cause mortality reductions in acute decompensated heart failure (23.5–26 kg/m2), HFpEF (21.7–31 kg/m2), HFrEF (21.7–43 kg/m2), females (24–25.5 kg/m2), diabetes (21.7–36 kg/m2), and non-diabetics (21.7–33 kg/m2).
Conclusion: Higher BMI is significantly associated with lower all-cause and cardiovascular mortality in patients with heart failure, supporting the presence of an obesity paradox. This protective effect was consistent across clinical subgroups, including HFpEF, HFrEF, males, females, and individuals with diabetes. The BMI paradox was evident in patients with acute decompensated heart failure, HFpEF, HFrEF, females, and both with and without diabetes.
Hypothesis: Higher BMI is associated with reduced mortality in patients with heart failure, and that this relationship varies across clinical subgroups and U-shaped relationship.
Methods: We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. A search strategy was developed, and studies were extracted from Cochrane and PubMed databases through December 2023. The main outcomes were all-cause mortality, cardiovascular deaths, and heart failure hospitalizations. Data were summarized as hazard ratios with 95% confidence intervals, and a spline model was used to assess non-linear relationships, with 21.7 kg/m2 as the reference point in the dose-response curve. PROSPERO: CRD42023455124
Results: Thirty-three studies (457,124 person-years) showed that each 5 kg/m2 increase in BMI was significantly associated with a 6% reduction in all-cause mortality (HR 0.94; 95% CI 0.92–0.96). Significant reductions were observed in acute decompensated heart failure (7%), HFpEF (9%), HFrEF (8%), diabetes (9%), males (9%), and females (8%). Cardiovascular mortality declined by 5% per 5 kg/m2 increase. Non-linear analysis revealed a significant U-shaped relationship, with lowest all-cause mortality between BMI 21.7 and 39 kg/m2. Subgroup analysis showed significant non-linear all-cause mortality reductions in acute decompensated heart failure (23.5–26 kg/m2), HFpEF (21.7–31 kg/m2), HFrEF (21.7–43 kg/m2), females (24–25.5 kg/m2), diabetes (21.7–36 kg/m2), and non-diabetics (21.7–33 kg/m2).
Conclusion: Higher BMI is significantly associated with lower all-cause and cardiovascular mortality in patients with heart failure, supporting the presence of an obesity paradox. This protective effect was consistent across clinical subgroups, including HFpEF, HFrEF, males, females, and individuals with diabetes. The BMI paradox was evident in patients with acute decompensated heart failure, HFpEF, HFrEF, females, and both with and without diabetes.
More abstracts on this topic:
A Cardiac Targeting Peptide Linked to miRNA106a Targets and Suppresses Genes Known to Cause Heart Failure: Reversing Heart Failure at the Source
Lu Ming, Deng Claire, Taskintuna Kaan, Ahern Gerard, Yurko Ray, Islam Kazi, Zahid Maliha, Gallicano Ian
A New Biomarker of Aging Derived From Electrocardiogram Improves Risk Prediction of Incident Myocardial Infarction and Stroke.Wilsgaard Tom, Rosamond Wayne, Schirmer Henrik, Lindekleiv Haakon, Attia Zachi, Lopez-jimenez Francisco, Leon David, Iakunchykova Olena