Final ID: Mo2045
Time-Sensitive Cardiovascular Risk After COVID-19: A Population-Based Study Across Variant Eras
Abstract Body (Do not enter title and authors here): Introduction
Cardiovascular risks following SARS-CoV-2 infection are incompletely defined. We evaluated evolving cardiovascular outcomes across COVID-19 variant eras using a large community-based cohort to inform risk stratification and clinical care.
Methods
We conducted a retrospective cohort study of 162,471 adults with COVID-19 between March 2020 and December 2023 using the Rochester Epidemiology Project. Patients were stratified by variant era (Pre-Delta, Delta, and Omicron). Cardiovascular outcomes included major adverse cardiovascular events (MACE: myocardial infarction, stroke, death), ischemic and inflammatory heart disease, thrombotic events, and dysrhythmias. Diagnoses were identified using ICD-10 codes and validated in a subset. Cumulative incidence was estimated using Kaplan-Meier and competing risk models. Cox proportional hazards regression was used to assess differences by era and age.
Results
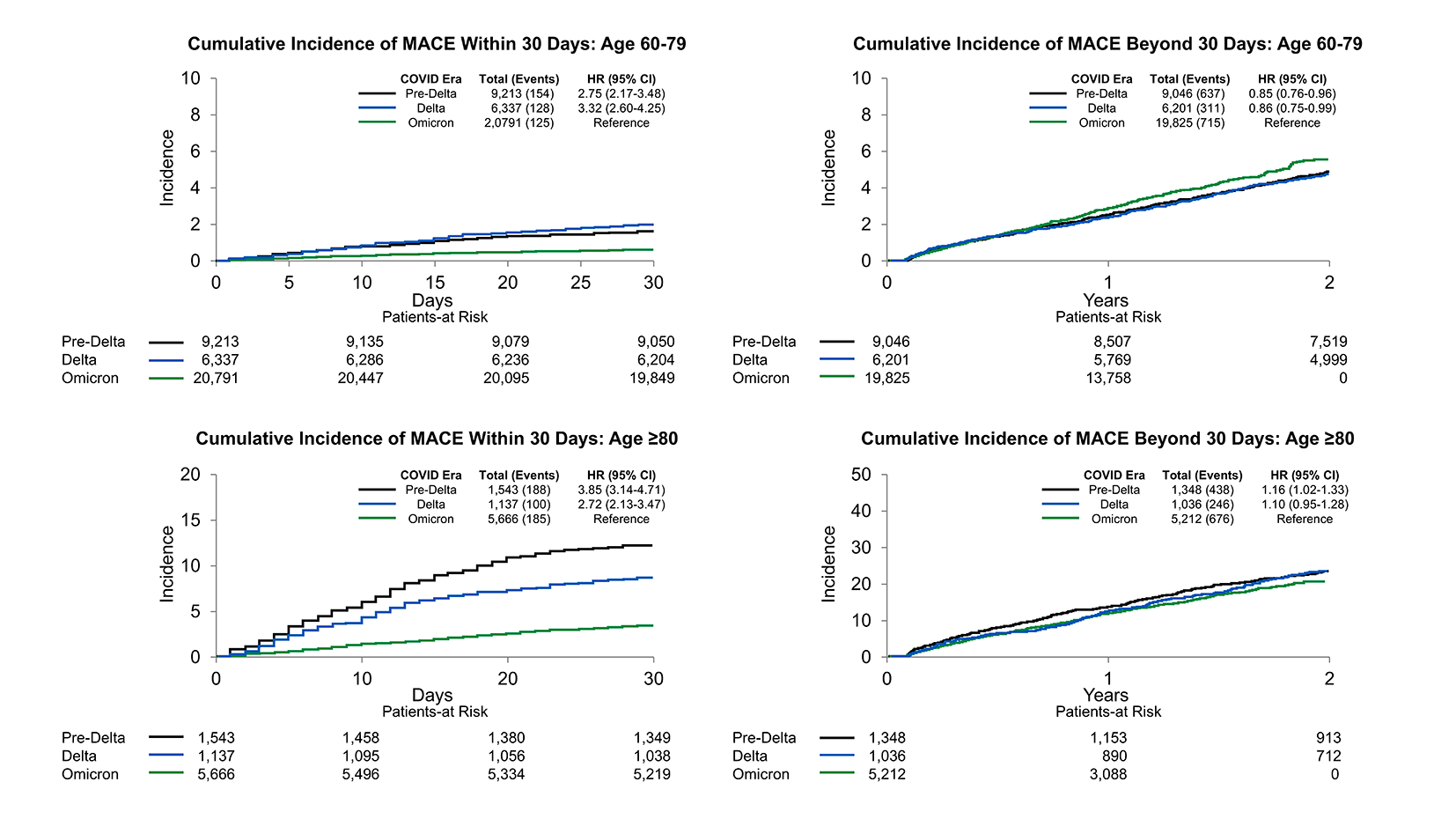
MACE occurred in 4,922 patients, primarily in those ≥80 (2-year incidence: 17%). Event rates peaked within 30 days post-infection, with marked variation by variant. In patients ≥80, 30-day MACE risk was highest in the Pre-Delta (HR 3.85; 95% CI, 3.14–4.71) and Delta (HR 2.72; 95% CI, 2.13–3.47) eras versus Omicron. After 30 days, event rates fell and era differences narrowed. Thrombotic events (n=2,090; 1.4%) decreased across eras. Ischemic and inflammatory heart disease rates were stable. Myocarditis/pericarditis were rare (0.1%) without age trends.
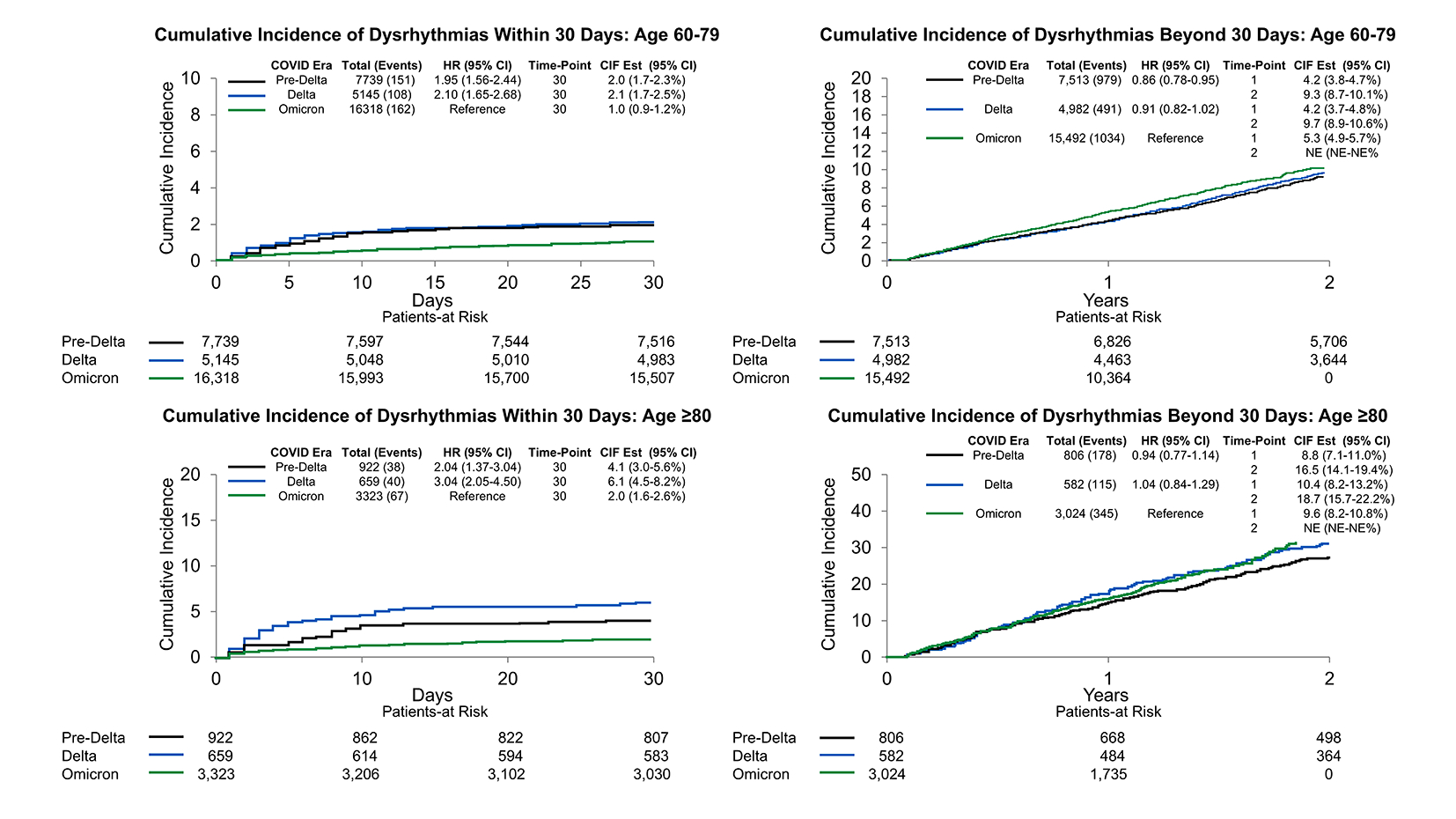
Dysrhythmias affected 6,765 patients (2-year incidence: 4.9%) and rose with age (2.0% in <40 vs. 19.9% in ≥80). Within 30 days, risk was higher in the Pre-Delta and Delta eras for age ≥40, especially ≥80 (Delta HR 3.08; 95% CI, 2.08–4.56) and 60–79 (HR 2.23; 95% CI, 1.75–2.85). Among those 40–59, Delta posed the highest risk (HR 2.74; 95% CI, 1.94–3.86 vs. Pre-Delta HR 1.77; 95% CI, 1.26–2.49). No differences were observed in <40. Beyond 30 days, risk converged across variants.
Conclusion
Cardiovascular risk after SARS-CoV-2 infection was concentrated in the first 30 days, with attenuation thereafter. While MACE and thrombotic event rates declined over time, early dysrhythmia risk varied by variant and age, especially in older adults. These findings define a time-sensitive, variant-specific risk window and support short-term, risk-stratified post-COVID monitoring. This work informs targeted follow-up protocols by infection era and age, with implications for quality improvement, resource use, and equitable care.
Cardiovascular risks following SARS-CoV-2 infection are incompletely defined. We evaluated evolving cardiovascular outcomes across COVID-19 variant eras using a large community-based cohort to inform risk stratification and clinical care.
Methods
We conducted a retrospective cohort study of 162,471 adults with COVID-19 between March 2020 and December 2023 using the Rochester Epidemiology Project. Patients were stratified by variant era (Pre-Delta, Delta, and Omicron). Cardiovascular outcomes included major adverse cardiovascular events (MACE: myocardial infarction, stroke, death), ischemic and inflammatory heart disease, thrombotic events, and dysrhythmias. Diagnoses were identified using ICD-10 codes and validated in a subset. Cumulative incidence was estimated using Kaplan-Meier and competing risk models. Cox proportional hazards regression was used to assess differences by era and age.
Results
MACE occurred in 4,922 patients, primarily in those ≥80 (2-year incidence: 17%). Event rates peaked within 30 days post-infection, with marked variation by variant. In patients ≥80, 30-day MACE risk was highest in the Pre-Delta (HR 3.85; 95% CI, 3.14–4.71) and Delta (HR 2.72; 95% CI, 2.13–3.47) eras versus Omicron. After 30 days, event rates fell and era differences narrowed. Thrombotic events (n=2,090; 1.4%) decreased across eras. Ischemic and inflammatory heart disease rates were stable. Myocarditis/pericarditis were rare (0.1%) without age trends.
Dysrhythmias affected 6,765 patients (2-year incidence: 4.9%) and rose with age (2.0% in <40 vs. 19.9% in ≥80). Within 30 days, risk was higher in the Pre-Delta and Delta eras for age ≥40, especially ≥80 (Delta HR 3.08; 95% CI, 2.08–4.56) and 60–79 (HR 2.23; 95% CI, 1.75–2.85). Among those 40–59, Delta posed the highest risk (HR 2.74; 95% CI, 1.94–3.86 vs. Pre-Delta HR 1.77; 95% CI, 1.26–2.49). No differences were observed in <40. Beyond 30 days, risk converged across variants.
Conclusion
Cardiovascular risk after SARS-CoV-2 infection was concentrated in the first 30 days, with attenuation thereafter. While MACE and thrombotic event rates declined over time, early dysrhythmia risk varied by variant and age, especially in older adults. These findings define a time-sensitive, variant-specific risk window and support short-term, risk-stratified post-COVID monitoring. This work informs targeted follow-up protocols by infection era and age, with implications for quality improvement, resource use, and equitable care.
More abstracts on this topic:
Double Trouble: Impact of Viral Pneumonia on Mortality and Clinical Outcomes in Patients Hospitalized with Pulmonary Embolism: A Nationwide Analysis (2016 – 2021)
Towfig Muhanned Faisal, Sule-saa Samuel, Akella Sai Anusha, Ahmed Mugtaba, Muriuki Hiram, Adedayo Ajibola
ISG15 is responsible for endothelial inflammation and vascular disfunction induced by Spike protein 1 of SARS-CoV-2.Rios Francisco, Montezano Augusto, Camargo Livia, Lopes Rheure, Garcia Ana, Aranday-cortes Elihu, Briones Ana, Mclauchlan John, Touyz Rhian