Final ID: MP631
Association of Hospital Shock Center Level with In-Hospital Outcomes in Cardiogenic Shock: An Analysis of the Nationwide Readmissions Database
Abstract Body (Do not enter title and authors here): Background: Patients with cardiogenic shock (CS) have high in-hospital mortality. Regionalized systems of care, modeled after trauma and ST-segment-elevation myocardial infarction networks, have been proposed to improve outcomes. Expert consensus frameworks classify CS centers based on mechanical circulatory support (MCS) capabilities, but national outcome data remain limited. This study assessed the association between hospital shock center designation and clinical outcomes.
Methods: Adults (≥18 y) hospitalized with a primary or secondary diagnosis of CS were identified from the Nationwide Readmissions Database (2016–2022). Hospitals were stratified annually into four CS center levels using procedural codes: Level 1 (≥1 durable left ventricular assist device or cardiac transplantation [LVAD/HTx] transplant case), Level 1A (extracorporeal membrane oxygenation, Impella 5.5 or TandemHeart capable without durable LVAD/HTx), Level 2 (percutaneous coronary intervention [PCI]-capable hospitals offering intra-aortic balloon pump [IABP] or Impella CP/RP), and Level 3 (non-PCI, non-MCS hospitals with ICU-level care only). Outcomes included in-hospital mortality, 30-day readmissions, MCS use, length of stay (LOS), and cost. Multinomial overlap propensity and hierarchical regression models were used to adjust and analyze outcomes.
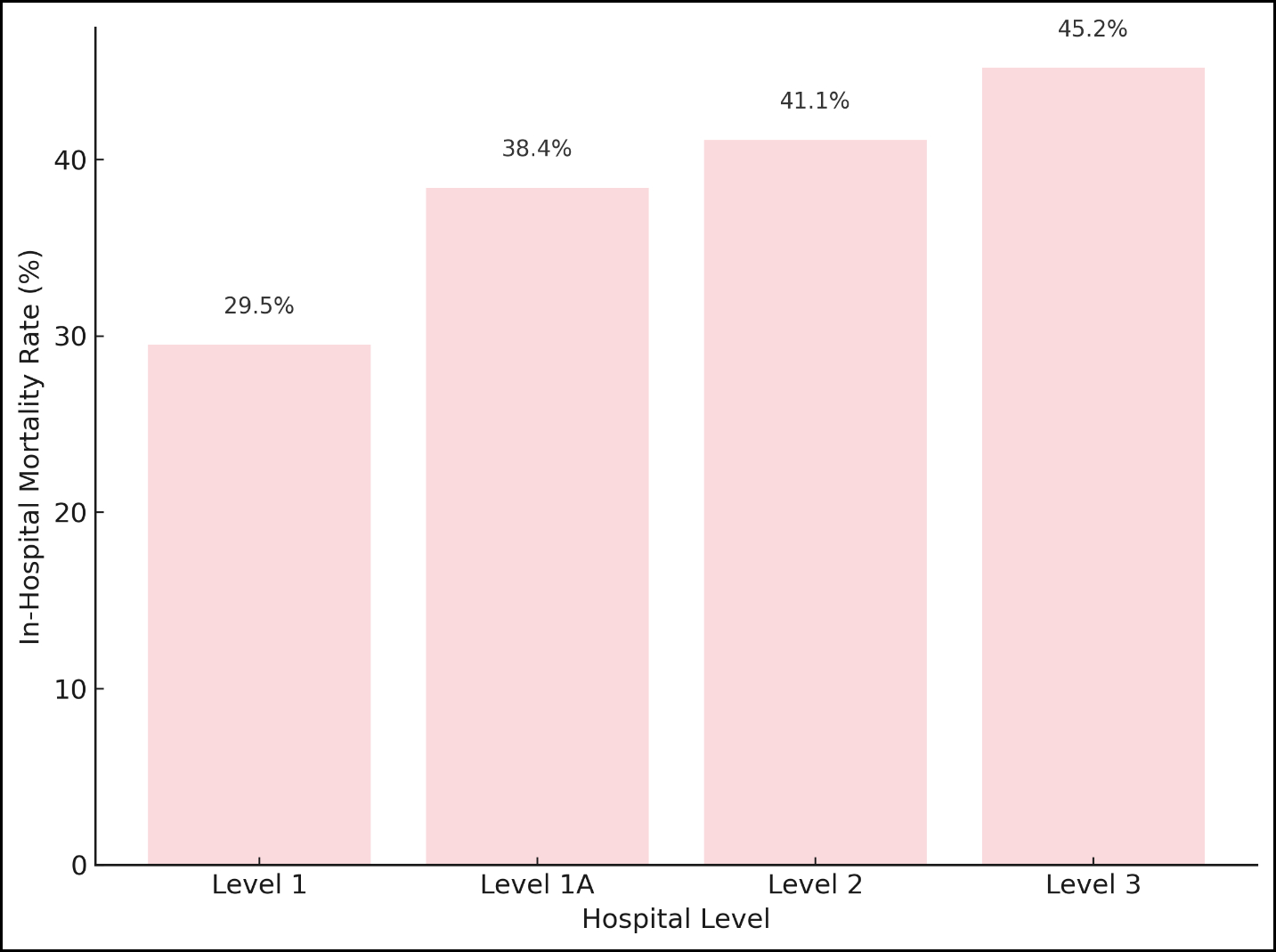
Results: Among 623,835 CS hospitalizations, 33.8% occurred at Level 1, 49.5% at Level 1A, 11.8% at Level 2, and 4.8% at Level 3 centers. After propensity weighting, baseline characteristics were well balanced across shock center levels. In-hospital mortality increased across levels: unadjusted 29.5% at Level 1, 38.4% at Level 1A, 41.1% at Level 2, and 45.2% at Level 3; adjusted analyses vs. Level 1: odds ratio 1.33 [95% CI, 1.29–1.38] for Level 1A; 1.44 [95% CI, 1.38–1.50] for Level 2; 1.63 [95% CI, 1.54–1.71] for Level 3; all p<0.001 (Figure 1). MCS use was highest at Level 1 centers (26.1%) and lowest at Level 2 centers (10.4%). Thirty-day readmission rates were lower at lower-level centers compared to Level 1. LOS and costs were highest at Level 1 centers. Pre-specified subgroup analyses showed consistent survival benefit favoring higher-level centers.
Conclusion: In a large national study, higher tiers of CS centers were associated with improved short-term outcomes independent of patient comorbidity and acuity supporting the need for regionalization of CS care.
Methods: Adults (≥18 y) hospitalized with a primary or secondary diagnosis of CS were identified from the Nationwide Readmissions Database (2016–2022). Hospitals were stratified annually into four CS center levels using procedural codes: Level 1 (≥1 durable left ventricular assist device or cardiac transplantation [LVAD/HTx] transplant case), Level 1A (extracorporeal membrane oxygenation, Impella 5.5 or TandemHeart capable without durable LVAD/HTx), Level 2 (percutaneous coronary intervention [PCI]-capable hospitals offering intra-aortic balloon pump [IABP] or Impella CP/RP), and Level 3 (non-PCI, non-MCS hospitals with ICU-level care only). Outcomes included in-hospital mortality, 30-day readmissions, MCS use, length of stay (LOS), and cost. Multinomial overlap propensity and hierarchical regression models were used to adjust and analyze outcomes.
Results: Among 623,835 CS hospitalizations, 33.8% occurred at Level 1, 49.5% at Level 1A, 11.8% at Level 2, and 4.8% at Level 3 centers. After propensity weighting, baseline characteristics were well balanced across shock center levels. In-hospital mortality increased across levels: unadjusted 29.5% at Level 1, 38.4% at Level 1A, 41.1% at Level 2, and 45.2% at Level 3; adjusted analyses vs. Level 1: odds ratio 1.33 [95% CI, 1.29–1.38] for Level 1A; 1.44 [95% CI, 1.38–1.50] for Level 2; 1.63 [95% CI, 1.54–1.71] for Level 3; all p<0.001 (Figure 1). MCS use was highest at Level 1 centers (26.1%) and lowest at Level 2 centers (10.4%). Thirty-day readmission rates were lower at lower-level centers compared to Level 1. LOS and costs were highest at Level 1 centers. Pre-specified subgroup analyses showed consistent survival benefit favoring higher-level centers.
Conclusion: In a large national study, higher tiers of CS centers were associated with improved short-term outcomes independent of patient comorbidity and acuity supporting the need for regionalization of CS care.
More abstracts on this topic:
A Simple One-Item Nursing Falls Assessment Predicts Outcomes For Patients With Stage D Heart Failure Undergoing Surgical Advanced Therapies
Salvador Vincent, Perez Jaime Abraham, Hudec Paige, Gorodeski Eiran, Oneill Thomas
A recombinant protein oxygen carrier with reduced nitric oxide scavenging as a blood substitute for resuscitationXu Qinzi, Rochon Elizabeth, Bocian Kaitlin, Huang Xue, Poropatich Ronald, Gladwin Mark, Tejero Jesus, Rose Jason, Rodriguez Deborah, Hwang Hyon, Turner Bryan, Hunt Thomas, Dent Matthew, Demartino Anthony, Abdelghany Youmna, Chen Xiukai