Final ID: MP2418
Impact of Diabetes and Glycemic Control on Cardiovascular Outcomes Following Left Atrial Appendage (LAA) Occlusion: A Propensity Matched Analysis.
Abstract Body (Do not enter title and authors here): Background:
Diabetes mellitus is a known risk factor for adverse cardiovascular outcomes, particularly in patients with atrial fibrillation. While left atrial appendage occlusion (LAAO) has emerged as a viable alternative to long-term anticoagulation, the influence of glycemic control on post-procedural outcomes remains inadequately defined. This study aimed to evaluate cardiovascular outcomes among nondiabetic (NDM), well-controlled diabetic (WCDM; HbA1c <7%), and poorly controlled diabetic (PCDM; HbA1c ≥7%) patients undergoing LAAO.
Research Question: Does diabetes and its glycemic control status affect adverse cardiovascular outcomes
following LAAO in atrial fibrillation patients?
Methods:
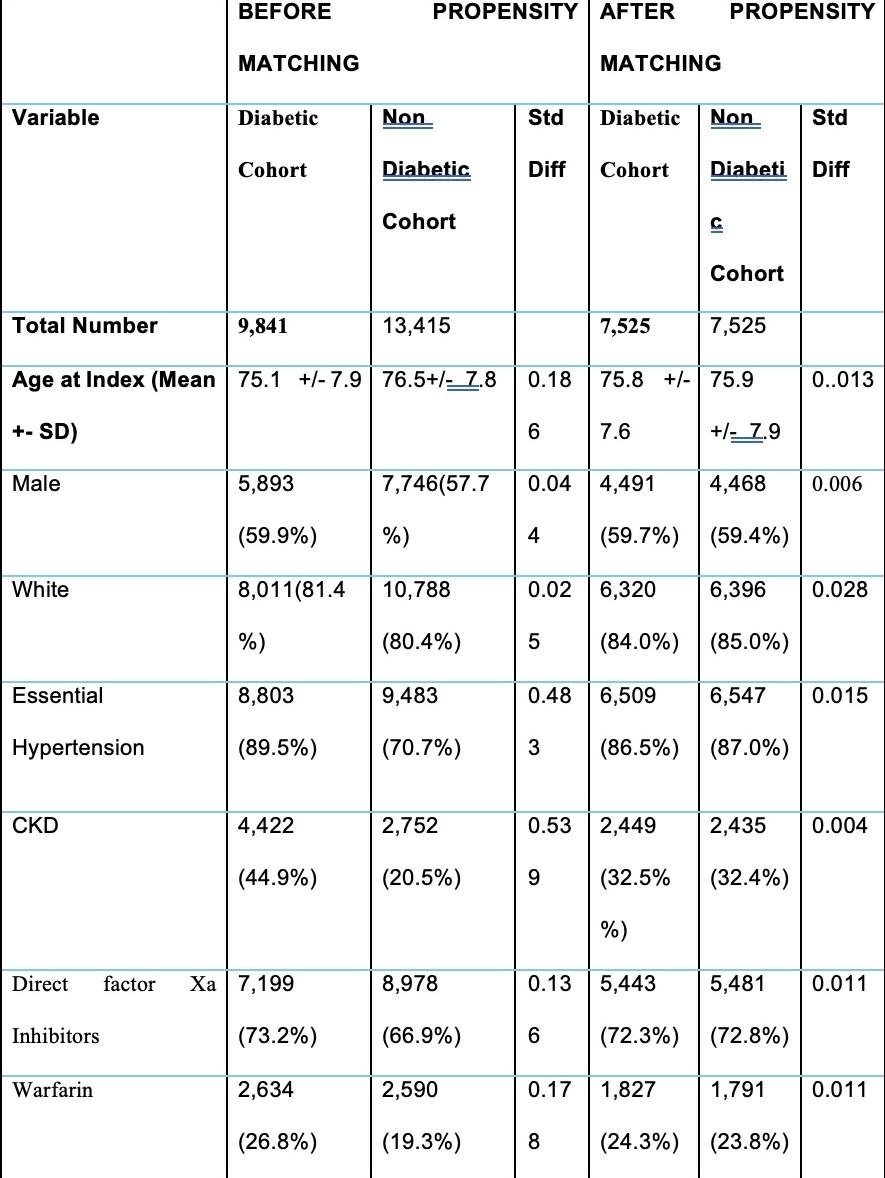
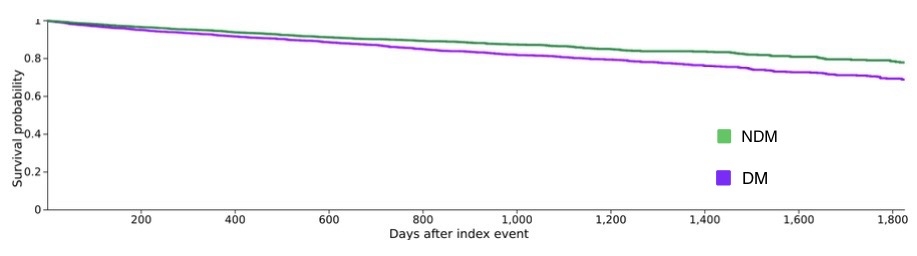
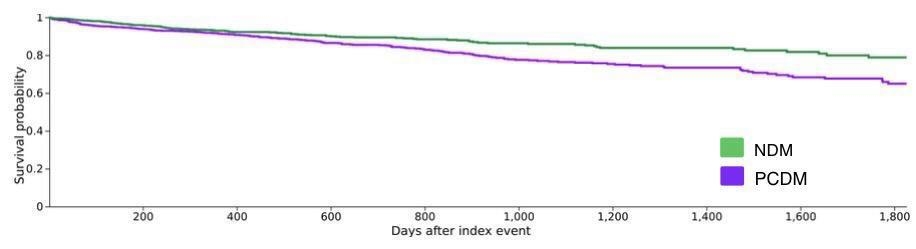
Using the TriNetX Global Collaborative Network, we identified adult AF patients who underwent LAAO between 2018 and 2024. Patients were stratified into three comparisons: Diabetics vs NDM, WCDM vs NDM, and PCDM vs NDM. Propensity score matching (PSM) was employed to balance 26 baseline covariates across cohorts. Outcomes including major adverse cardiovascular events (MACE), stroke and all-cause mortality were assessed over a 5-year follow-up. Risk analysis and Kaplan-Meier survival curves were used to derive hazard ratios (HR) and 95% confidence intervals (CI).
Results:
In the overall analysis, major adverse cardiovascular events (MACE) occurred in 13.4% of diabetics versus 9.0% of non-diabetics (HR, 1.44; 95% CI, 1.28–1.62) and all-cause mortality in 15.2% versus 12.3% (HR, 1.15; 95% CI, 1.05–1.25). Stroke occurred in 5.1% versus 3.6% (HR, 1.30; 95% CI, 1.09–1.54), pulmonary embolism in 2.8% versus 2.1% (HR, 1.25; 95% CI, 1.02–1.54), and ventricular fibrillation in 1.0% versus 0.5% (HR, 1.81; 95% CI, 1.22–2.70). In the HbA1c >7% subgroup, MACE risk was further elevated (HR, 1.59; 95% CI, 1.25–2.00), whereas diabetics with HbA1c <7% still experienced increased risk (HR, 1.39; 95% CI, 1.21–1.60) compared with non-diabetics.
Conclusion:
Poor glycemic control (HbA1c ≥7%) in diabetic patients with atrial fibrillation undergoing LAAO is associated with a significantly increased long-term risk of MACE, stroke, and mortality. Notably, both suboptimal and even controlled glycemic states appear to confer elevated cardiovascular risk, underscoring the complex interplay between diabetes and outcomes post-LAAO. These findings highlight the critical importance of individualized glycemic management and comprehensive cardiovascular risk reduction strategies in this high-risk population.
Diabetes mellitus is a known risk factor for adverse cardiovascular outcomes, particularly in patients with atrial fibrillation. While left atrial appendage occlusion (LAAO) has emerged as a viable alternative to long-term anticoagulation, the influence of glycemic control on post-procedural outcomes remains inadequately defined. This study aimed to evaluate cardiovascular outcomes among nondiabetic (NDM), well-controlled diabetic (WCDM; HbA1c <7%), and poorly controlled diabetic (PCDM; HbA1c ≥7%) patients undergoing LAAO.
Research Question: Does diabetes and its glycemic control status affect adverse cardiovascular outcomes
following LAAO in atrial fibrillation patients?
Methods:
Using the TriNetX Global Collaborative Network, we identified adult AF patients who underwent LAAO between 2018 and 2024. Patients were stratified into three comparisons: Diabetics vs NDM, WCDM vs NDM, and PCDM vs NDM. Propensity score matching (PSM) was employed to balance 26 baseline covariates across cohorts. Outcomes including major adverse cardiovascular events (MACE), stroke and all-cause mortality were assessed over a 5-year follow-up. Risk analysis and Kaplan-Meier survival curves were used to derive hazard ratios (HR) and 95% confidence intervals (CI).
Results:
In the overall analysis, major adverse cardiovascular events (MACE) occurred in 13.4% of diabetics versus 9.0% of non-diabetics (HR, 1.44; 95% CI, 1.28–1.62) and all-cause mortality in 15.2% versus 12.3% (HR, 1.15; 95% CI, 1.05–1.25). Stroke occurred in 5.1% versus 3.6% (HR, 1.30; 95% CI, 1.09–1.54), pulmonary embolism in 2.8% versus 2.1% (HR, 1.25; 95% CI, 1.02–1.54), and ventricular fibrillation in 1.0% versus 0.5% (HR, 1.81; 95% CI, 1.22–2.70). In the HbA1c >7% subgroup, MACE risk was further elevated (HR, 1.59; 95% CI, 1.25–2.00), whereas diabetics with HbA1c <7% still experienced increased risk (HR, 1.39; 95% CI, 1.21–1.60) compared with non-diabetics.
Conclusion:
Poor glycemic control (HbA1c ≥7%) in diabetic patients with atrial fibrillation undergoing LAAO is associated with a significantly increased long-term risk of MACE, stroke, and mortality. Notably, both suboptimal and even controlled glycemic states appear to confer elevated cardiovascular risk, underscoring the complex interplay between diabetes and outcomes post-LAAO. These findings highlight the critical importance of individualized glycemic management and comprehensive cardiovascular risk reduction strategies in this high-risk population.
More abstracts on this topic:
Bioresponsive Liposomal Nanoparticle-based Co-Delivery of tPA and DNase I Lyses tPA-Resistant Neutrophil Extracellular-Rich Clots
Raghunathan Shruti, Disharoon Dante, Hu Keren, Wang Hanyang, Hernandez Selvin, Sen Gupta Anirban
A novel risk score predicts the prevalence of left atrial low-voltage areas and rhythm outcome in patients undergoing long-standing persistent atrial fibrillation ablationOoka Hirotaka, Nakao Sho, Kusuda Masaya, Ariyasu Wataru, Kudo Satoshi, Fujii Subaru, Mano Toshiaki, Matsuda Yasuhiro, Masuda Masaharu, Okamoto Shin, Ishihara Takayuki, Nanto Kiyonori, Tsujimura Takuya, Hata Yosuke, Uematsu Hiroyuki