Final ID: MP1779
Utilization of Advanced Diagnostics in Younger Adults with First Unexplained Ventricular Tachycardia, Ventricular Fibrillation or Cardiac: A U.S. Based Multicenter Cohort Study
Abstract Body (Do not enter title and authors here): Background
Current studies evaluating diagnostic testing in younger adults with first ventricular fibrillation (VF), tachycardia (VT) or cardiac arrest is largely limited to tertiary centers or designated registries, with few reflecting community practices. Variation in the diagnostic workup for younger adults with first ventricular tachyarrhythmias may lead to under-recognition of treatable or preventable underlying conditions.
Research Question
In the real-world setting, how are advanced diagnostics utilized in adult patients under 60 years-old with first VF, VT, or cardiac arrest, and what are the diagnostic yields?
Methods
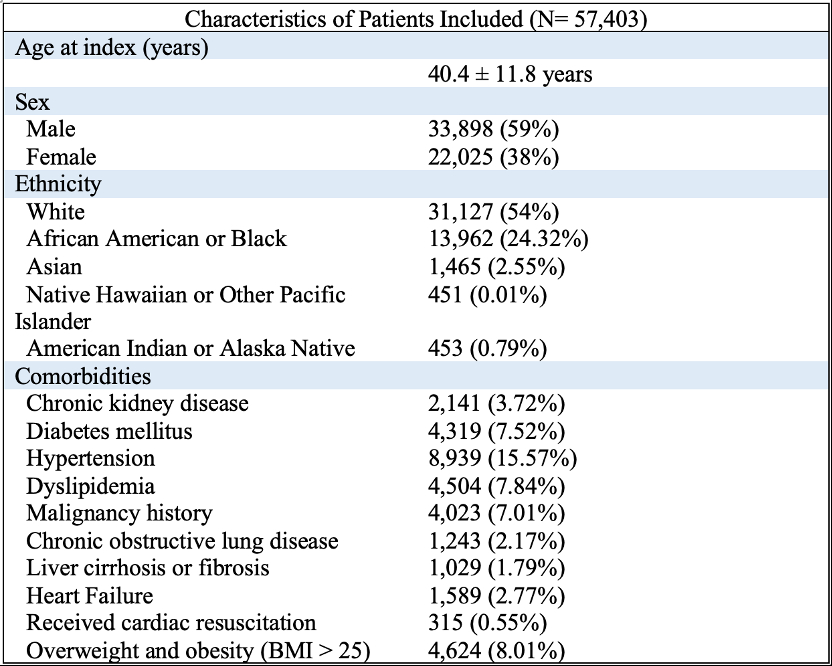
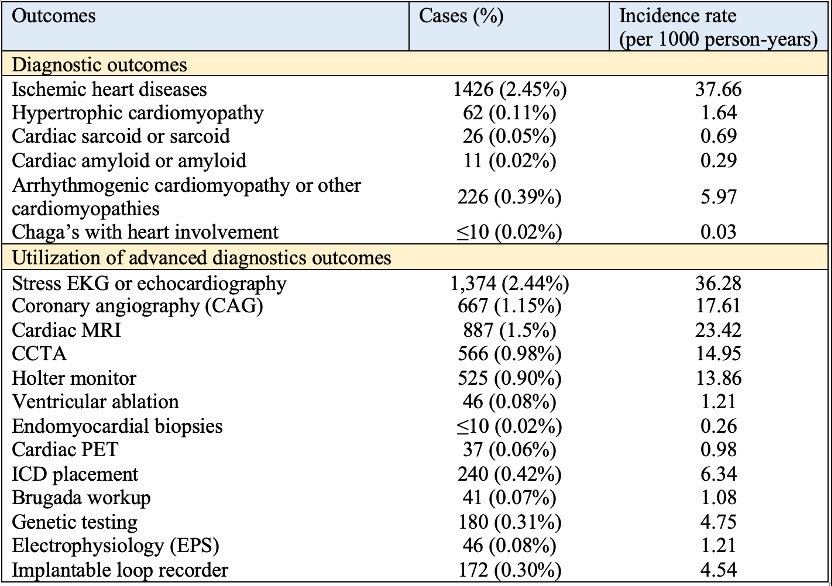
Using a U.S.-based multicenter retrospective database (TriNetX), adults (18 - 60 years), with first VF, VT or cardiac arrest (2019 to 2024) were included (Table 1). Patients with prior implantable cardioverter-defibrillator or pacemakers, ischemic cardiomyopathy, amyloidosis, sarcoidosis, or hypertrophic cardiomyopathy (HCM) were excluded. Outcomes were utilization rates for coronary angiography (CAG), CCTA, cardiac MRI, cardiac PET, myocardial biopsy, genetic testing, exercise ECGs, electrophysiological testing, implantable loop recorder, and diagnostic yield of cardiomyopathies (e.g. sarcoidosis, amyloidosis, HCM, or other channelopathies). Incidence rates were calculated using mean person-time over a 5-year period.
Results
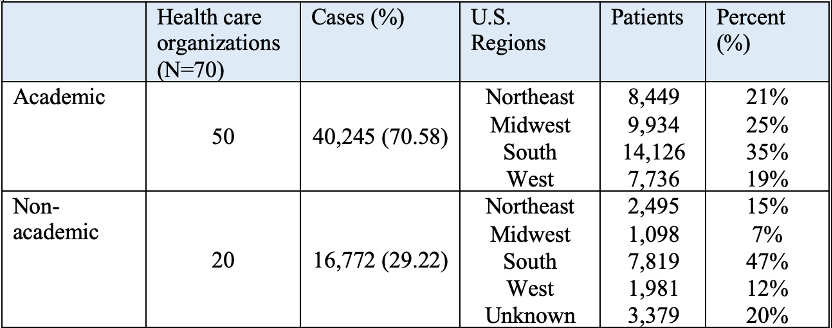
A total of 57,403 patients were included, 40,245 (71%) received care at academic institutions. Mean follow-up was 237.70 ± 436.36 days, median follow-up 9 days (IQR: 276 days), totaling 37,310 person-years. The mean age of was 40.4 ± 11.8 years. In these patients, 1,374 (2.44%) received stress EKG or echocardiogram, 887 patients (1.5%) cardiac MRI, 556 (0.98%) CCTA, 180 (0.31%) genetic testing, and 172 (0.30%) received implantable loop recorder evaluation. For diagnostic outcomes, only 1,426 (2.45%) were diagnosed with ischemic heart disease, 226 (0.39%) arrhythmogenic cardiomyopathy or other cardiomyopathies, 62 (0.11%) HCM, 26 (0.05%) with sarcoidosis (Table 2). Incidence rates are presented in Table 2; regional distribution as presented in Table 3.
Conclusions
In a large national cohort, advanced diagnostic workups were infrequently performed in younger adults with first ventricular tachyarrhythmias. The brief median follow-up time suggests poor continuity in the real-world setting. This underscores the need for standardized and systemic evaluation pathways to improve outcomes and treat preventable conditions.
Current studies evaluating diagnostic testing in younger adults with first ventricular fibrillation (VF), tachycardia (VT) or cardiac arrest is largely limited to tertiary centers or designated registries, with few reflecting community practices. Variation in the diagnostic workup for younger adults with first ventricular tachyarrhythmias may lead to under-recognition of treatable or preventable underlying conditions.
Research Question
In the real-world setting, how are advanced diagnostics utilized in adult patients under 60 years-old with first VF, VT, or cardiac arrest, and what are the diagnostic yields?
Methods
Using a U.S.-based multicenter retrospective database (TriNetX), adults (18 - 60 years), with first VF, VT or cardiac arrest (2019 to 2024) were included (Table 1). Patients with prior implantable cardioverter-defibrillator or pacemakers, ischemic cardiomyopathy, amyloidosis, sarcoidosis, or hypertrophic cardiomyopathy (HCM) were excluded. Outcomes were utilization rates for coronary angiography (CAG), CCTA, cardiac MRI, cardiac PET, myocardial biopsy, genetic testing, exercise ECGs, electrophysiological testing, implantable loop recorder, and diagnostic yield of cardiomyopathies (e.g. sarcoidosis, amyloidosis, HCM, or other channelopathies). Incidence rates were calculated using mean person-time over a 5-year period.
Results
A total of 57,403 patients were included, 40,245 (71%) received care at academic institutions. Mean follow-up was 237.70 ± 436.36 days, median follow-up 9 days (IQR: 276 days), totaling 37,310 person-years. The mean age of was 40.4 ± 11.8 years. In these patients, 1,374 (2.44%) received stress EKG or echocardiogram, 887 patients (1.5%) cardiac MRI, 556 (0.98%) CCTA, 180 (0.31%) genetic testing, and 172 (0.30%) received implantable loop recorder evaluation. For diagnostic outcomes, only 1,426 (2.45%) were diagnosed with ischemic heart disease, 226 (0.39%) arrhythmogenic cardiomyopathy or other cardiomyopathies, 62 (0.11%) HCM, 26 (0.05%) with sarcoidosis (Table 2). Incidence rates are presented in Table 2; regional distribution as presented in Table 3.
Conclusions
In a large national cohort, advanced diagnostic workups were infrequently performed in younger adults with first ventricular tachyarrhythmias. The brief median follow-up time suggests poor continuity in the real-world setting. This underscores the need for standardized and systemic evaluation pathways to improve outcomes and treat preventable conditions.
More abstracts on this topic:
Antisense Oligonucleotide Treatment of Calmodulinopathy
Bortolin Raul, Yoshinaga Daisuke, Pavlaki Nikoleta, Cavazzoni Cecilia B., T. Sage Peter, D. Whitehill Robert, Abrams Dominic, Carreon Chrystalle, Putra Juan, Alexandrescu Sanda, Guo Shuai, Nawar Farina, Tsai Owen, Rubart Michael, Kubli Dieter, Mullick Adam, Bezzerides Vassilios, Pu William, Trembley Michael, Prondzynski Maksymilian, Sweat Mason, Wang Peizhe, Chaehyoung Park, Lu Fujian, Keating Erin
A Heart-pounding Case of Cardiomyopathy in PregnancyTran Linh, Everitt Ian, Vaught Arthur, Barth Andreas, Minhas Anum