Final ID: MP2648
Anti-Arrhythmic drugs versus Catheter Ablation Prognostic value in the patients with Diastolic Heart Failure and Atrial Fibrillation: a Systematic Review and Meta-analysis of 38,237 Patients
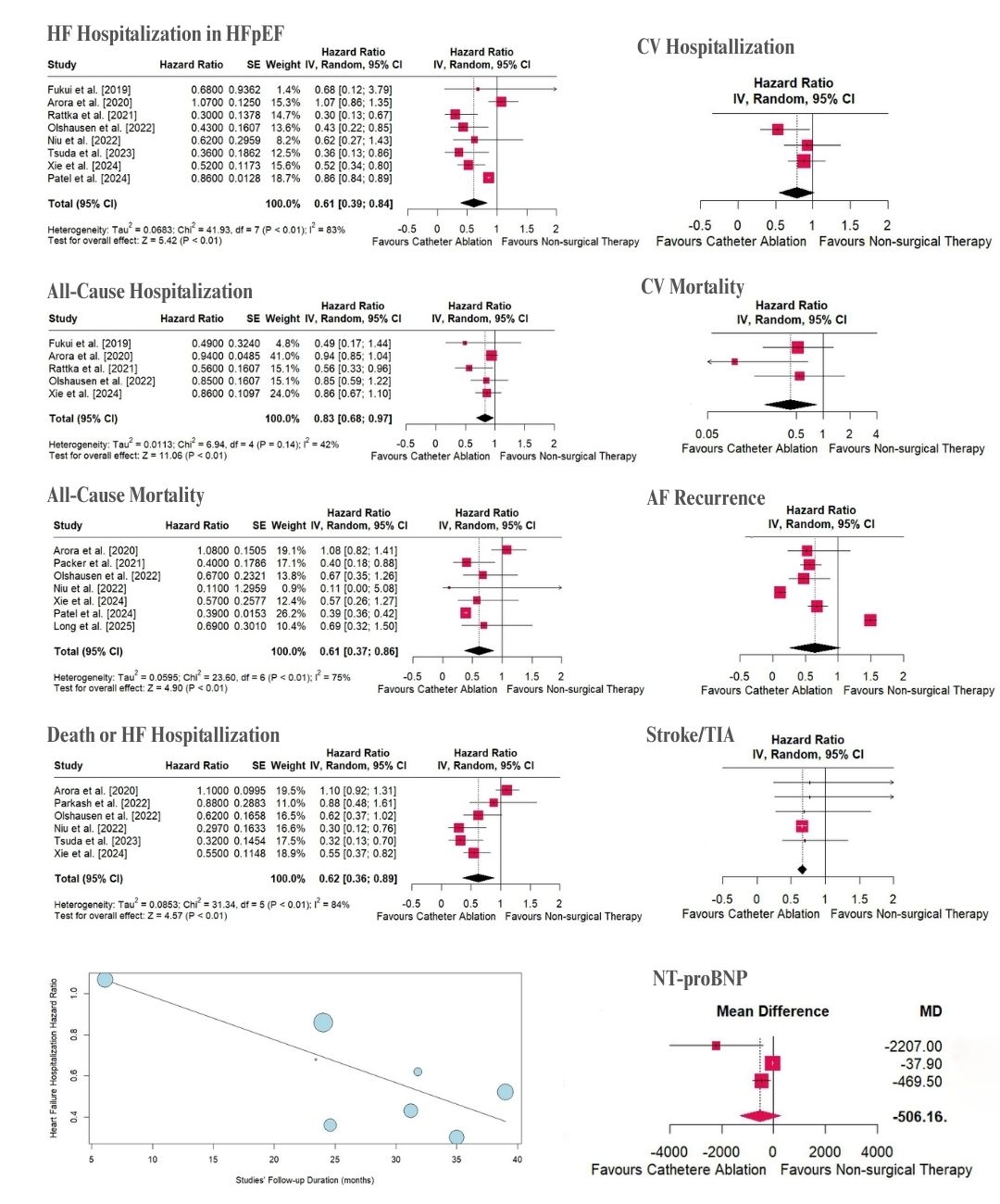
Abstract Body (Do not enter title and authors here): Background: There is no definite consensus on the best treatment option for atrial fibrillation (AF) in heart failure (HF) with preserved ejection fraction (HFpEF) population. Aim: This study aims to systematically review the prognostic effects of catheter ablation (CA) in patients with HFpEF and AF and provide quantitative pooled analysis where applicable. Methods: A systematic search of PubMed/Medline, Web of Science, Embase, ClinicalTrials.gov, Cochrane, Scopus, and Google Scholar was conducted for observational and randomized clinical trial studies on HFpEF patients published up to March 15, 2025. Studies were included if they evaluated the clinical prognostic utility for CA in AF patients with at least 6 months of follow-up. Pooled estimates and 95% CI for CA hazard ratio (HR) or mean difference (MD)/standardized MD (SMD) in each outcome were calculated using a random effects model by RStudio 2025.05.1 software. Results: Twelve studies with 38,237 participants (mean age 69.6) underwent descriptive analysis, and 11 eligible studies were included in the meta-analysis. CA was associated with a lower risk of HF hospitalization (HR: 0.61, 95% CI: 0.39-0.84, I2: 83%, p<0.01), cardiovascular (CV) hospitalization (HR: 0.78, 95% CI: 0.55-1.01, I2: 42%, p<0.01), all-cause hospitalization (HR: 0.83, 95% CI: 0.68-0.97, I2: 42%, p<0.01), CV mortality (HR: 0.43, 95% CI: 0.22-0.84, I2: 22%, p:0.01), and all-cause mortality (HR: 0.61, 95% CI: 0.37-0.86, I2: 75%, p<0.01). Similarly, the risk for composite outcome (death or HF hospitalization; HR: 0.62, 95% CI: 0.36-0.89, I2: 84%, p<0.01), AF recurrence (HR: 0.64, 95% CI: 0.26-1.03, I2: 99%, p<0.01), and stroke/transient ischemic (TIA) attacks (HR: 0.66, 95% CI: 0.59-0.73, I2: 0%, p<0.01) decreased significantly in the CA group. Moreover, CA was linked to a statistically significant decrease in NT-proBNP level (MD: -500.16; SMD: -0.53, 95% CI: -0.71 to -0.35, I2: 0%, p<0.01) and a clinically negligible increase in ejection fraction (MD: 5.34; SMD: 0.4, 95% CI: 0.21-0.59, I2: 0%, p<0.01). Meta-regression results showed that CA was associated with greater long-term reduction in HF hospitalization, with risk decreasing over time compared to the usual anti-arrhythmic drugs approach, which can suggest the reverse remodeling potential of CA in the long term. Conclusion: The results indicated that CA is linked with better prognosis in the patients with HFpEF and AF, with more prominent benefits in long-term follow-ups.
More abstracts on this topic:
A new genetic model organism for primate-specific cardiac function and disease
Chang Stephen, Albertelli Megan, Quertermous Thomas, Wright Patricia, Terrien Jeremy, Aujard Fabienne, Wu Joseph, Krasnow Mark, Karanewsky Caitlin, Pendleton Jozeph, Ren Lu, Anzeraey Aude, Froelicher Victor, Liang David, Razafindrakoto Andriamahery, Ravelonjanahary Noeline
1-Year Outcomes After Cardioversion With and Without Anticoagulation in Patients With Left Atrial Appendage Occlusion: A Propensity-Matched AnalysisThangjui Sittinun, Trongtorsak Angkawipa, Kewcharoen Jakrin, Thyagaturu Harshith, Watson Hangyu, Mensah Samuel, Balla Sudarshan, Navaravong Leenhapong