Final ID: MDP1488
Prognostic Significance of Echocardiographic Transaortic Flow Rate in Aortic Valve Stenosis: a Systematic Review and Meta-Analysis
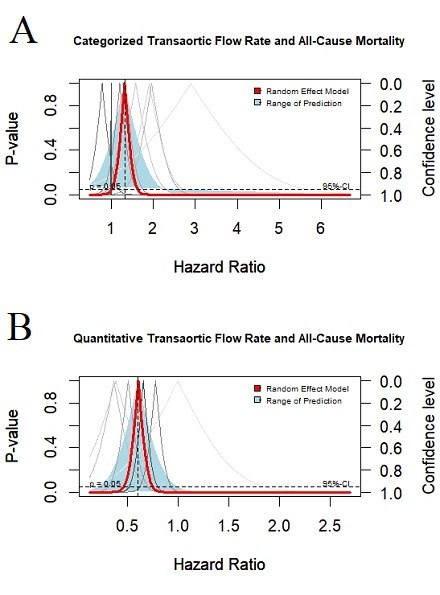
Abstract Body (Do not enter title and authors here): Background: Echocardiographic evaluation of Aortic valve stenosis (AS) severity relies on aortic valve area, peak jet velocity, and mean transaortic gradient. In pursuit of improving accuracy, the transaortic flow rate (FR), defined as the ratio of stroke volume to systolic ejection time, has been introduced. However, its prognostic value in AS patients remains controversial. Aim: This study aims to systematically review the predictive value of FR in AS patients and provide quantitative pooled analysis results where applicable. Methods: A systematic search of PubMed/Medline, Embase, Scopus, Web of Science, and Cochrane was conducted for observational studies on AS patients published up to March 15, 2024. Studies were included if they assessed the clinical prognostic utility of FR with at least three months of follow-up. Pooled estimates and 95% CI for FR's hazard ratio (HR) in each binary outcome were calculated using a random effects model. Results: Nineteen studies with 9456 patients (mean age 75) underwent descriptive analysis, and 17 eligible studies were included in the meta-analysis. For predicting all-cause mortality, the pooled HR for low FR measured at rest (cut-off value 200-210 mL/s) was 1.32 (95% CI: 1.01–1.63, I2: 69%, p<0.05) (Figure 1. A). For FR measured during stress echocardiography, the pooled HR was higher at 1.58 (95% CI: 1.20–1.96, I2: 0%, p<0.05). Additionally, every 100 mL/s increase in FR significantly reduced all-cause mortality; the HR was 0.61 (95% CI: 0.47–0.75, I2: 47%) for FR measured at rest (Figure 1. B), and 0.61 (95% CI: 0.31–0.91, I2: 65%) for FR measured during stress echo. For the combined endpoint of mortality and hospitalization, the HRs were as follows: 2.54 (95% CI: -0.99–6.08, I2: 48%) and 2.57 (95% CI: 0.69–4.44, I2: 0%) for the low FR group at rest and during stress echo, respectively. For every 100 mL/s increase in FR, the HRs were 0.19 (95% CI: -0.19–0.58, I2: 61%) at rest and 0.36 (95% CI: 0.18–0.54, I2: 0%) during stress echo. Conclusion: FR is a prognostic marker for all-cause mortality in AS patients, indicating its potential for risk stratification. Incorporating FR into clinical assessments could help personalize follow-up and monitoring strategies.
More abstracts on this topic:
2 Dimensional Echocardiography versus 3 Dimentional Echocardiography to Assess Right Ventricular Function in Pulmonary Hypertension: A Systematic Review
Chaudhry Waleed Razzaq, Hajj Fatima, Bathula Satyamedha, Meghji Mohammed Askari, Pasupuleti Hemalatha, Kiyani Madiha, Shah Syeda Simrah, Neelakantan Ramaswamy Sanathanan, Mirzaeidizaji Nakisa, St. Jacques Jahnoy, Khan Khalil Ullah, Veluchamy Elakkiya, Jesse Joshanna
Association Between Myocardial Lipomatous Metaplasia And Sudden Cardiac Death In Patients With Prior Myocardial InfarctionAisikaier Kaisaierjiang