Final ID: Su3003
Branch vs septum: A meta analysis of ventricular synchrony in Left bundle branch pacing vs left ventricular septal pacing with subgroup analysis based on baseline LVEF.
Abstract Body (Do not enter title and authors here): INTRODUCTION
Novel pacing methods including left bundle branch pacing(LBBP) and left ventricular septal pacing(LVSP) are being used to improve ventricular conduction and synchronization in patients with pacemakers. LBBP directly stimulates the left bundle branch, whereas LVSP paces the left ventricular septum. Key electrophysiological markers for assessing ventricular synchrony include left ventricular activation time(LVAT), paced QRS duration(pQRS), and delta QRS, which is defined as the change in QRS duration from intrinsic to paced rhythm.
GOAL
This systematic review & meta-analysis compares LVAT, pQRS duration, and delta QRS between LBBP and LVSP along with subgroup analysis by preserved(LVEF≥50%) versus reduced(LVEF<50%) baseline LVEF, providing insights into their potential clinical implications.
METHODS
We systematically searched major databases(PubMed, Embase..) for English-language studies involving patients requiring permanent pacing and reporting at least one relevant outcome. 12 studies met inclusion criteria. Data were pooled using the inverse variance method with a random-effects model in R statistical Studio.
Results
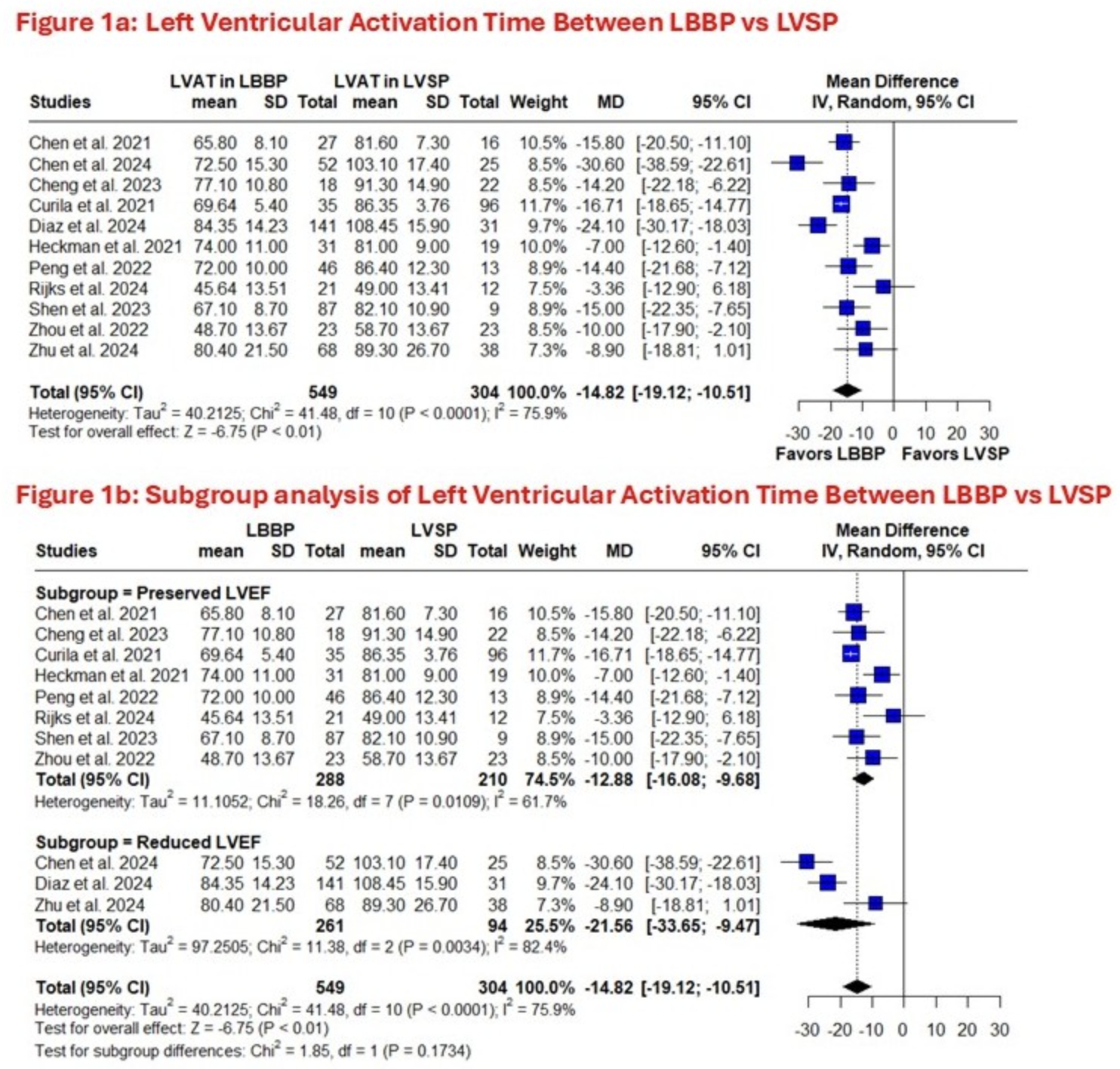
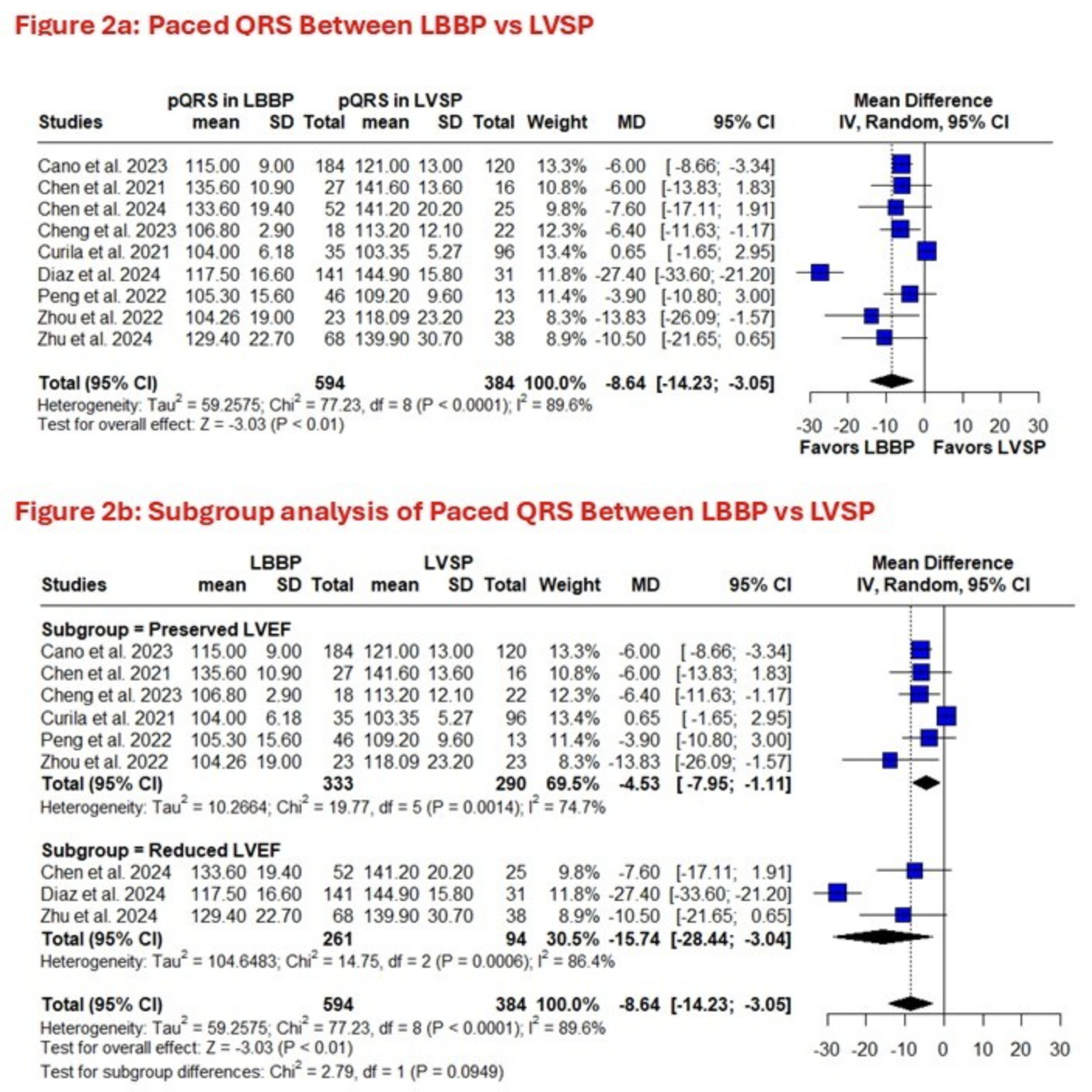
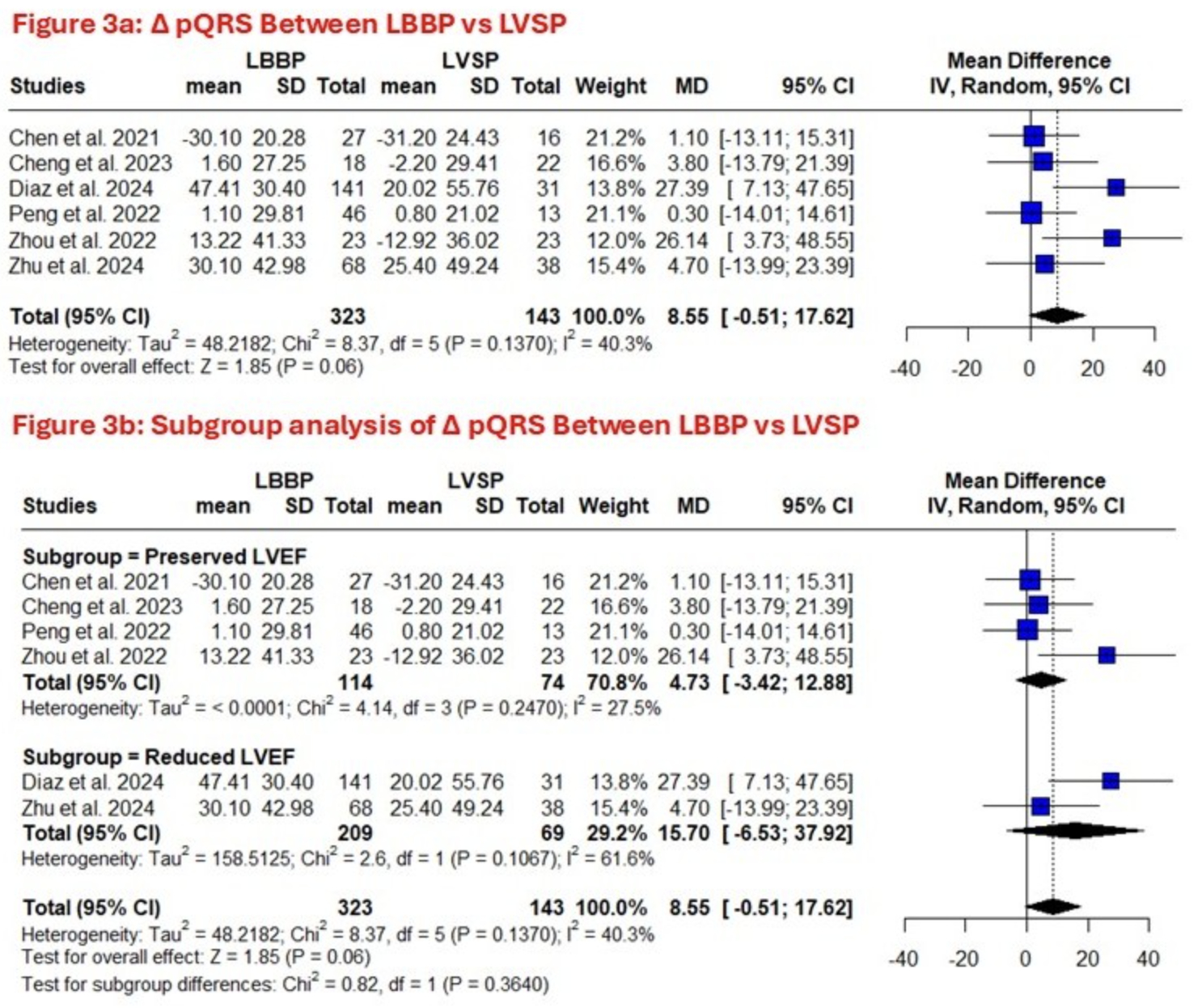
Meta analysis of 12 studies comprising 1157 patients showed that Compared to LVSP, LBBP significantly improved electrical synchrony with shorter LVAT(MD –14.82 ms,CI –19.12 to –10.51,p<0.001), lower pQRS(MD –8.64 ms,CI –14.23 to –3.05,p=0.002), and increased ΔQRS(MD –10.19 ms,CI –20.11 to -0.27,p=0.04). Subgroup analysis revealed LBBP substantially decreased LVAT in both preserved and reduced LVEF cohorts(MD –12.88 ms,p<0.001 & MD –21.56 ms,p=0.001,interaction p=0.17). LBBP also substantially lowered pQRS length in preserved and reduced LVEF patients(MD –4.53 ms,p=0.009 & –15.74 ms,p=0.020,interaction p=0.095). In ΔQRS, LBBP was preferred overall, but subgroup analyses for preserved and reduced LVEF were non-significant(MD –7.11 ms,p=0.21 & MD –15.79 ms,p=0.16), presumably due to limited power. Primary analyses demonstrated moderate heterogeneity.
Conclusion
LBBP significantly optimizes electrical ventricular synchrony over LVSP, evidenced by shorter LVAT and narrower pQRS durations. Patients with reduced baseline LVEF, have numerically greater effects than preserved LVEF, though subgroup interactions were not statistically significant. Findings support LBBP as a preferred strategy for achieving physiological pacing across the LVEF spectrum. Further research on long-term clinical outcomes and optimal lead placement is warranted.
Novel pacing methods including left bundle branch pacing(LBBP) and left ventricular septal pacing(LVSP) are being used to improve ventricular conduction and synchronization in patients with pacemakers. LBBP directly stimulates the left bundle branch, whereas LVSP paces the left ventricular septum. Key electrophysiological markers for assessing ventricular synchrony include left ventricular activation time(LVAT), paced QRS duration(pQRS), and delta QRS, which is defined as the change in QRS duration from intrinsic to paced rhythm.
GOAL
This systematic review & meta-analysis compares LVAT, pQRS duration, and delta QRS between LBBP and LVSP along with subgroup analysis by preserved(LVEF≥50%) versus reduced(LVEF<50%) baseline LVEF, providing insights into their potential clinical implications.
METHODS
We systematically searched major databases(PubMed, Embase..) for English-language studies involving patients requiring permanent pacing and reporting at least one relevant outcome. 12 studies met inclusion criteria. Data were pooled using the inverse variance method with a random-effects model in R statistical Studio.
Results
Meta analysis of 12 studies comprising 1157 patients showed that Compared to LVSP, LBBP significantly improved electrical synchrony with shorter LVAT(MD –14.82 ms,CI –19.12 to –10.51,p<0.001), lower pQRS(MD –8.64 ms,CI –14.23 to –3.05,p=0.002), and increased ΔQRS(MD –10.19 ms,CI –20.11 to -0.27,p=0.04). Subgroup analysis revealed LBBP substantially decreased LVAT in both preserved and reduced LVEF cohorts(MD –12.88 ms,p<0.001 & MD –21.56 ms,p=0.001,interaction p=0.17). LBBP also substantially lowered pQRS length in preserved and reduced LVEF patients(MD –4.53 ms,p=0.009 & –15.74 ms,p=0.020,interaction p=0.095). In ΔQRS, LBBP was preferred overall, but subgroup analyses for preserved and reduced LVEF were non-significant(MD –7.11 ms,p=0.21 & MD –15.79 ms,p=0.16), presumably due to limited power. Primary analyses demonstrated moderate heterogeneity.
Conclusion
LBBP significantly optimizes electrical ventricular synchrony over LVSP, evidenced by shorter LVAT and narrower pQRS durations. Patients with reduced baseline LVEF, have numerically greater effects than preserved LVEF, though subgroup interactions were not statistically significant. Findings support LBBP as a preferred strategy for achieving physiological pacing across the LVEF spectrum. Further research on long-term clinical outcomes and optimal lead placement is warranted.
More abstracts on this topic:
A Case Report of Cardiac Tamponade due to Mycoplasma Pneumoniae-induced Pericarditis - A Rare Complication of a Commonly seen Bacterial Infection
Patel Vidhi, Maharjan Reeju, Okan Tetyana, Singh Bhupinder, Colasacco Joseph
A New Biomarker of Aging Derived From Electrocardiogram Improves Risk Prediction of Incident Myocardial Infarction and Stroke.Wilsgaard Tom, Rosamond Wayne, Schirmer Henrik, Lindekleiv Haakon, Attia Zachi, Lopez-jimenez Francisco, Leon David, Iakunchykova Olena