Final ID: MP2637
Comparative Effectiveness and Safety of Left Atrial Appendage Occlusion Devices: A Comprehensive Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Background:
Percutaneous left atrial appendage occlusion (LAAO) is increasingly utilized for stroke prevention in non-valvular atrial fibrillation (NVAF) patients with contraindications to long-term anticoagulation. With growing global use of WATCHMAN, Amplatzer Amulet, and LAmbre devices, a comprehensive comparison integrating randomized controlled trials (RCTs) and real-world evidence is warranted.
Methods:
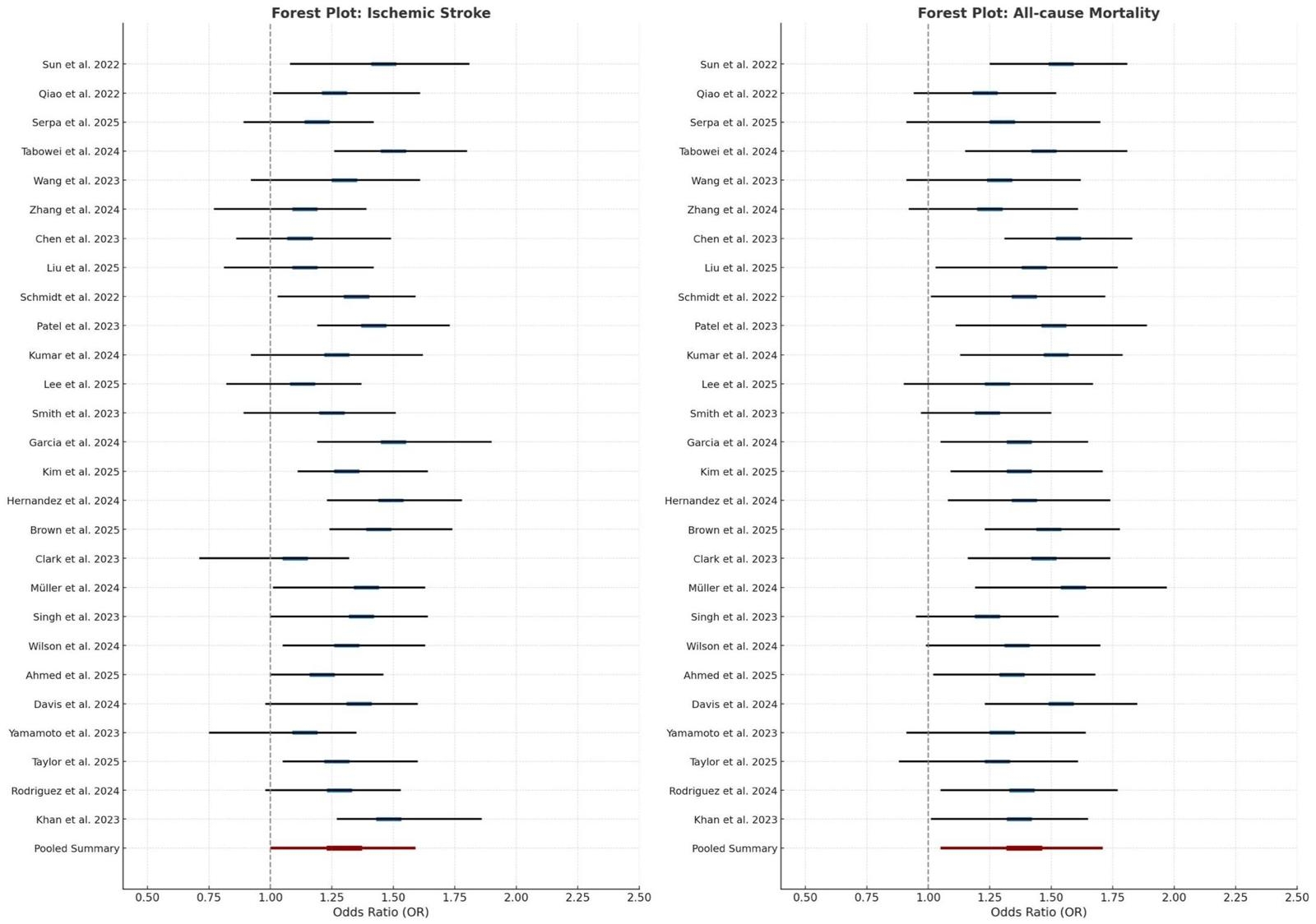
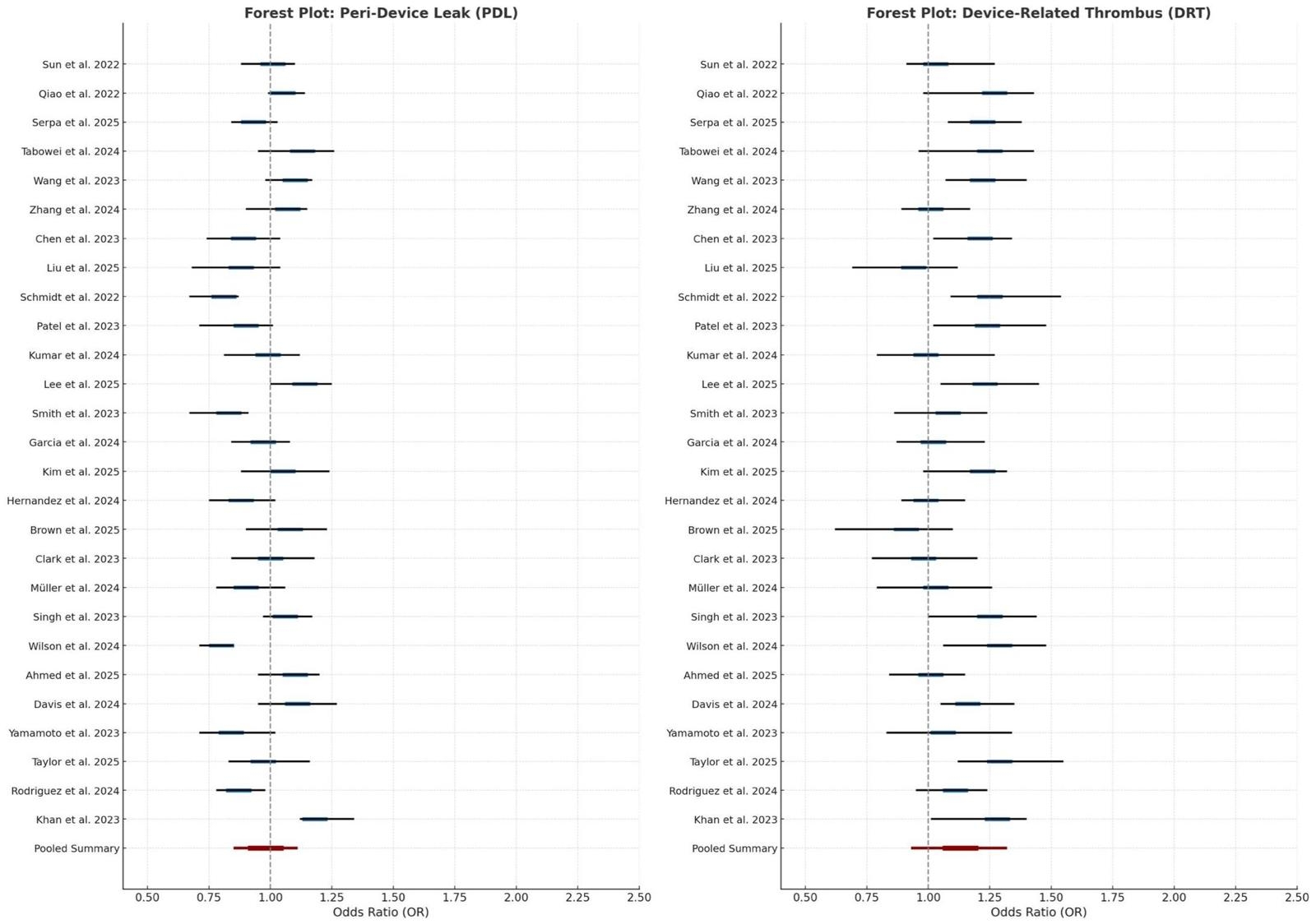
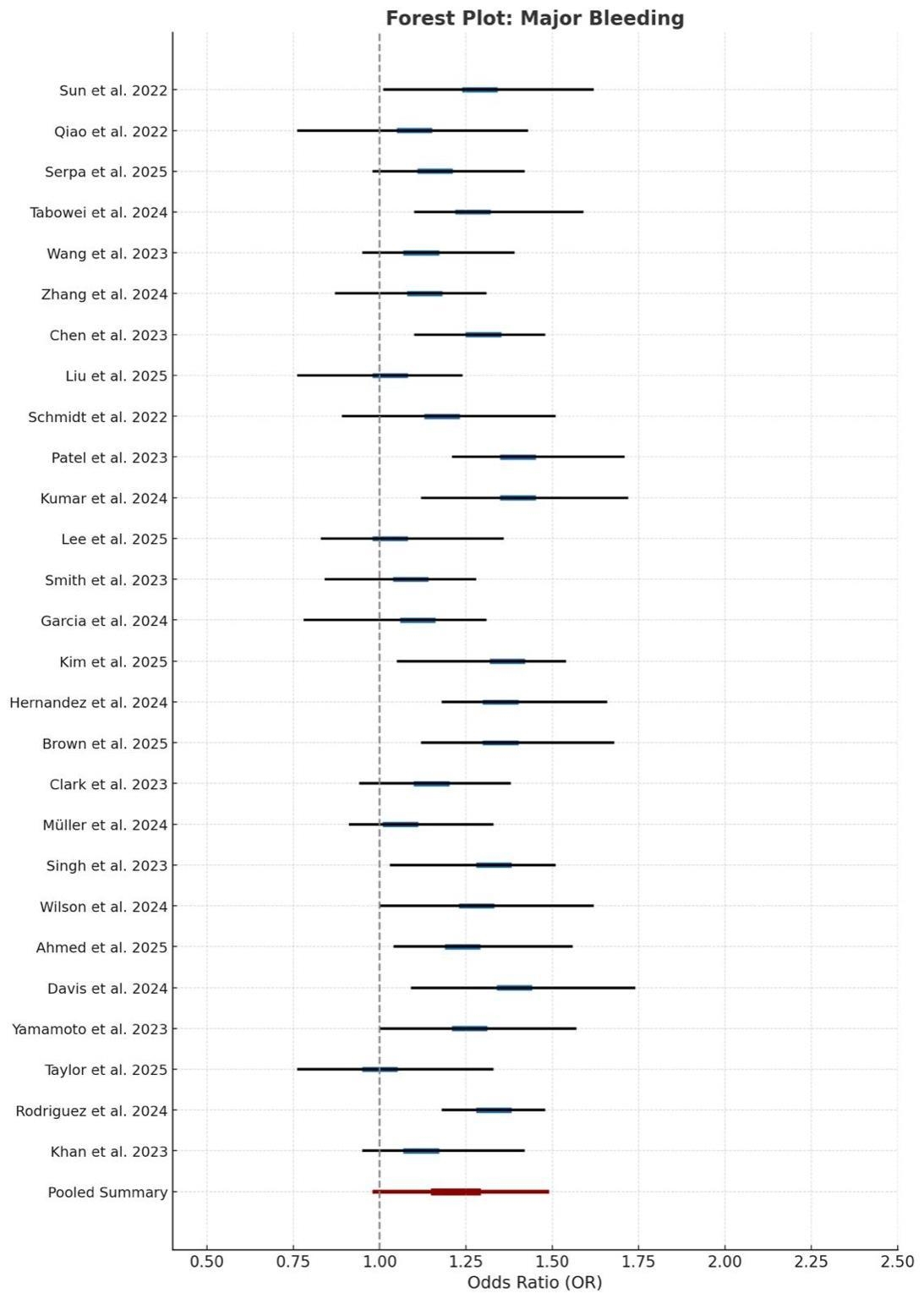
We conducted a systematic review and meta-analysis of RCTs, registries, and observational studies from PubMed, Scopus, Embase, and Cochrane (through June 2025), including studies reporting outcomes for WATCHMAN (2.5 and FLX), Amplatzer Amulet, and LAmbre. Primary endpoints included ischemic stroke, systemic embolism, all-cause mortality, major bleeding, device-related thrombus (DRT), peri-device leak (PDL), and procedural complications. Subgroup analyses assessed device type, CHADS2-VASc score, imaging modality (ICE vs TEE), and LAA anatomy. Random-effects models pooled trial and real-world data.
Results:
We analyzed 27 studies (12 RCTs, 15 observational; 65,308 patients). Procedural success exceeded 97% across devices. Annual ischemic stroke rates were 1.5% (WATCHMAN), 1.4% (Amulet), and 1.2% (LAmbre) (p=NS); all-cause mortality was 3.6%, 3.5%, and 3.3%, respectively. Major bleeding rates were 3.0% (WATCHMAN), 2.7% (Amulet), and 2.8% (LAmbre), with WATCHMAN FLX significantly reducing bleeding vs WATCHMAN 2.5 (OR 0.68, 95% CI 0.49–0.92). DRT occurred in 1.9% (WATCHMAN), 1.3% (Amulet), and 0.9% (LAmbre). Significant PDL (>5 mm) was highest with WATCHMAN (3.2%), lower with Amulet (1.1%) and LAmbre (0.7%). Device embolization occurred in 0.5% (Amulet), 0.2% (WATCHMAN), and 0% (LAmbre), while pericardial effusion rates were 3.1%, 2.8%, and 1.5%, respectively. ICE guidance improved procedural success (OR 1.11, 95% CI 1.03–1.21) but increased pericardial effusion risk (OR 1.22, 95% CI 1.05–1.42) vs TEE. Efficacy was consistent across CHADS2-VASc scores (mean 3.8 ± 1.3). LAmbre demonstrated superior adaptability in complex anatomies, including large ostia (≥31 mm), bilobed morphologies, and persistent thrombus.
Conclusion:
LAAO devices are safe and effective for stroke prevention in NVAF, with device-specific differences. Real-world data highlight LAmbre’s suitability for complex anatomies and Amulet’s lower leak rates. Optimal outcomes depend on individualized device selection based on anatomy, imaging, and bleeding risk.
Percutaneous left atrial appendage occlusion (LAAO) is increasingly utilized for stroke prevention in non-valvular atrial fibrillation (NVAF) patients with contraindications to long-term anticoagulation. With growing global use of WATCHMAN, Amplatzer Amulet, and LAmbre devices, a comprehensive comparison integrating randomized controlled trials (RCTs) and real-world evidence is warranted.
Methods:
We conducted a systematic review and meta-analysis of RCTs, registries, and observational studies from PubMed, Scopus, Embase, and Cochrane (through June 2025), including studies reporting outcomes for WATCHMAN (2.5 and FLX), Amplatzer Amulet, and LAmbre. Primary endpoints included ischemic stroke, systemic embolism, all-cause mortality, major bleeding, device-related thrombus (DRT), peri-device leak (PDL), and procedural complications. Subgroup analyses assessed device type, CHADS2-VASc score, imaging modality (ICE vs TEE), and LAA anatomy. Random-effects models pooled trial and real-world data.
Results:
We analyzed 27 studies (12 RCTs, 15 observational; 65,308 patients). Procedural success exceeded 97% across devices. Annual ischemic stroke rates were 1.5% (WATCHMAN), 1.4% (Amulet), and 1.2% (LAmbre) (p=NS); all-cause mortality was 3.6%, 3.5%, and 3.3%, respectively. Major bleeding rates were 3.0% (WATCHMAN), 2.7% (Amulet), and 2.8% (LAmbre), with WATCHMAN FLX significantly reducing bleeding vs WATCHMAN 2.5 (OR 0.68, 95% CI 0.49–0.92). DRT occurred in 1.9% (WATCHMAN), 1.3% (Amulet), and 0.9% (LAmbre). Significant PDL (>5 mm) was highest with WATCHMAN (3.2%), lower with Amulet (1.1%) and LAmbre (0.7%). Device embolization occurred in 0.5% (Amulet), 0.2% (WATCHMAN), and 0% (LAmbre), while pericardial effusion rates were 3.1%, 2.8%, and 1.5%, respectively. ICE guidance improved procedural success (OR 1.11, 95% CI 1.03–1.21) but increased pericardial effusion risk (OR 1.22, 95% CI 1.05–1.42) vs TEE. Efficacy was consistent across CHADS2-VASc scores (mean 3.8 ± 1.3). LAmbre demonstrated superior adaptability in complex anatomies, including large ostia (≥31 mm), bilobed morphologies, and persistent thrombus.
Conclusion:
LAAO devices are safe and effective for stroke prevention in NVAF, with device-specific differences. Real-world data highlight LAmbre’s suitability for complex anatomies and Amulet’s lower leak rates. Optimal outcomes depend on individualized device selection based on anatomy, imaging, and bleeding risk.
More abstracts on this topic:
A Delayed Diagnosis of Anti-HMG-CoA Reductase Immune-Mediated Necrotizing Myopathy
Jadhav Reshma, Shekar Arush, Westenhaver Zack, Skandhan Amith
A novel approach for LV delay evaluation: non-invasive QLV measurement using UHF ECGPoviser Lukas, Stros Petr, Vesela Jana, Curila Karol