Final ID: MP615
Tackling Telemetry: A Resident Run Initiative to Reduce Unnecessary Telemetry Use
Abstract Body (Do not enter title and authors here): Background: Telemetry is a valuable tool for close clinical monitoring. However, when used in non-indicated settings, it contributes to alarm fatigue, increased healthcare costs, and reduced patient satisfaction. Many studies have shown that unnecessary telemetry use does not improve clinical outcomes. Even when initially indicated, telemetry orders often remain active for longer than necessary.
Research Question: Will an educational intervention reduce inappropriate telemetry orders on admission and improve reassessment of telemetry after 48 hours?
Goals: Educate admitting hospitalists and internal medicine residents about American Heart Association (AHA) guidelines for telemetry in order to reduce unnecessary use.
Methods: We designed a quality improvement study using a pre-post analysis to measure the effect of education on telemetry use. Telemetry orders upon admission to a tertiary care center were analyzed by two physicians based on the 2017 AHA Best Practice guidelines. Orders were re-evaluated at 48 hours to assess whether telemetry remained indicated or was discontinued appropriately. Education regarding the AHA guidelines was then given to internal medicine residents and the non-teaching hospitalist service. After education, telemetry orders were again analyzed over a two week period. Results were analyzed for significance with a chi-square test using a p-value of significance set to 0.05.
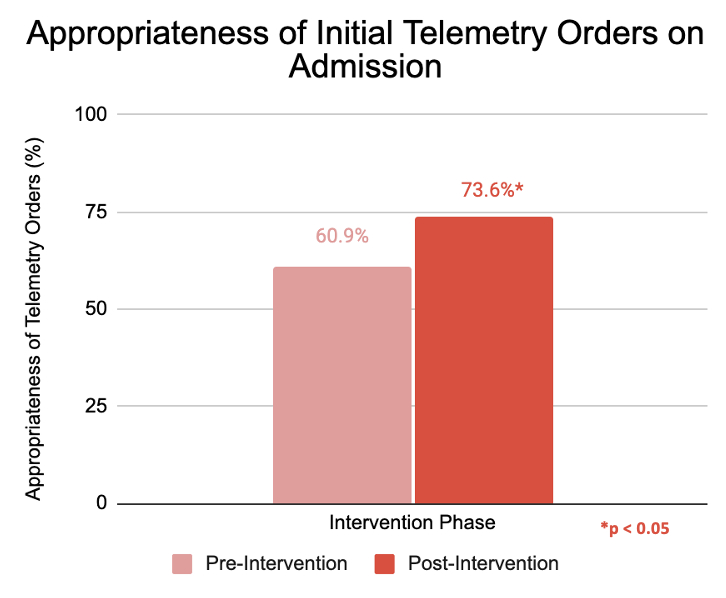
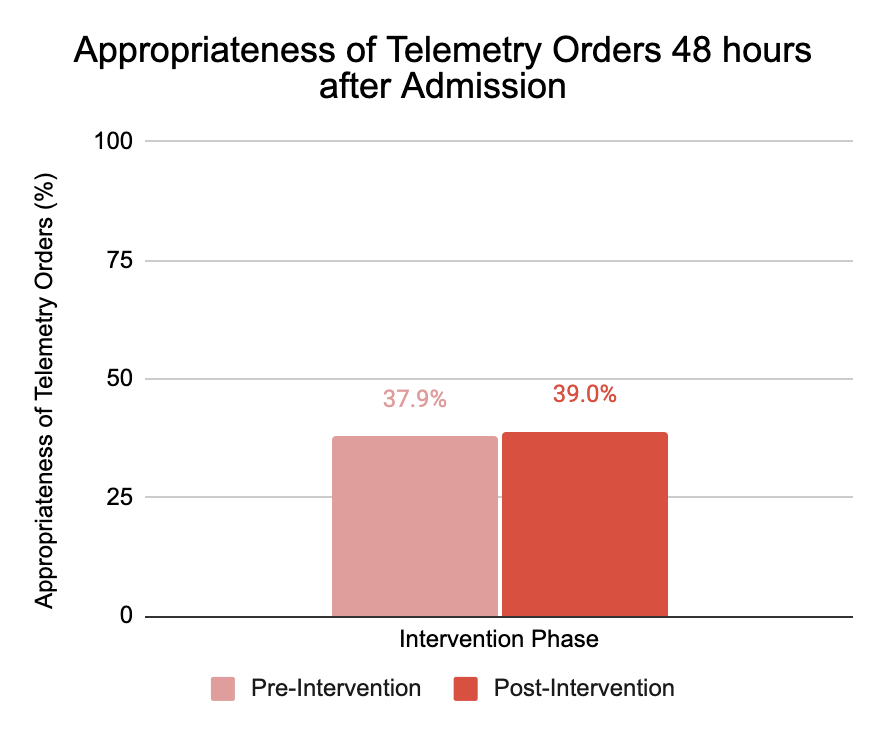
Results: Prior to the educational intervention, 156 admissions were analyzed. Following the intervention, 110 admissions were analyzed. The proportion of appropriate telemetry orders at admission significantly increased from 60.9% to 73.6% (p=0.03; 95% CI: 1.5%–23.9%) (Figure 1). No significant change was observed in appropriateness at 48 hours with 37.9% and 39% of orders deemed appropriate pre and post-education, respectively (p=1.00; 95% CI: -17.0% to 19.2%) (Figure 2).
Conclusion: Our study not only assessed telemetry upon admission but also uniquely re-evaluated use 48 hours later, highlighting an overlooked contributor to overuse. While an educational intervention improved initial ordering practices, it did not significantly impact ongoing telemetry reassessment or timely discontinuation. A future intervention to consider is additional electronic medical record advisories to improve telemetry orders after 48 hours. Future works should investigate the frequency of repeated education required to maintain high level ordering practices.
Research Question: Will an educational intervention reduce inappropriate telemetry orders on admission and improve reassessment of telemetry after 48 hours?
Goals: Educate admitting hospitalists and internal medicine residents about American Heart Association (AHA) guidelines for telemetry in order to reduce unnecessary use.
Methods: We designed a quality improvement study using a pre-post analysis to measure the effect of education on telemetry use. Telemetry orders upon admission to a tertiary care center were analyzed by two physicians based on the 2017 AHA Best Practice guidelines. Orders were re-evaluated at 48 hours to assess whether telemetry remained indicated or was discontinued appropriately. Education regarding the AHA guidelines was then given to internal medicine residents and the non-teaching hospitalist service. After education, telemetry orders were again analyzed over a two week period. Results were analyzed for significance with a chi-square test using a p-value of significance set to 0.05.
Results: Prior to the educational intervention, 156 admissions were analyzed. Following the intervention, 110 admissions were analyzed. The proportion of appropriate telemetry orders at admission significantly increased from 60.9% to 73.6% (p=0.03; 95% CI: 1.5%–23.9%) (Figure 1). No significant change was observed in appropriateness at 48 hours with 37.9% and 39% of orders deemed appropriate pre and post-education, respectively (p=1.00; 95% CI: -17.0% to 19.2%) (Figure 2).
Conclusion: Our study not only assessed telemetry upon admission but also uniquely re-evaluated use 48 hours later, highlighting an overlooked contributor to overuse. While an educational intervention improved initial ordering practices, it did not significantly impact ongoing telemetry reassessment or timely discontinuation. A future intervention to consider is additional electronic medical record advisories to improve telemetry orders after 48 hours. Future works should investigate the frequency of repeated education required to maintain high level ordering practices.
More abstracts on this topic:
Cardiology Conferences Have a Higher Research Yield Than Other Subspecialties: A 10-Year Follow-Up Study of AHA and ACC Annual Meetings
Rajani Aayushi, Patel Chinmay, Gandhi Devisha, Amin Juhi, Vaishnav Riya, Shah Navya, Karatela Shifa, Shah Purav, Bhuptani Hitanshi, Shah Krish, Desai Bhavi, Shah Dev, Soni Atman, Mittal Shreya
A New Biomarker of Aging Derived From Electrocardiogram Improves Risk Prediction of Incident Myocardial Infarction and Stroke.Wilsgaard Tom, Rosamond Wayne, Schirmer Henrik, Lindekleiv Haakon, Attia Zachi, Lopez-jimenez Francisco, Leon David, Iakunchykova Olena