Final ID: Sa2182
Adverse Social Determinants of Health in a Low-Income Population Hospitalized with Heart Failure
Abstract Body (Do not enter title and authors here): Background: Heart failure (HF) is a leading cause of hospitalization and readmission. Understanding the burden and impact of social determinants of health (SDOH) among HF patients at safety-net hospitals is critical for improving outcomes.
Methods: We conducted a prospective, cross-sectional study to identify the prevalence of adverse SDOH among patients hospitalized with acute HF at an urban, safety-net hospital. English or Spanish-speaking patients hospitalized for HF were enrolled between 11/2022-6/2023. We collected data across 5 SDOH domains based on the Healthy People 2030 SDOH Model from the U.S. Department of Health and Human Services. The overall burden of adverse SDOH parameters and their association with hospitalization or emergency room (ER) visits at 90 days was assessed. Multivariate logistic regression models adjusted for selected covariates from the total pool of demographic, clinical, and social covariates using stepwise regression.
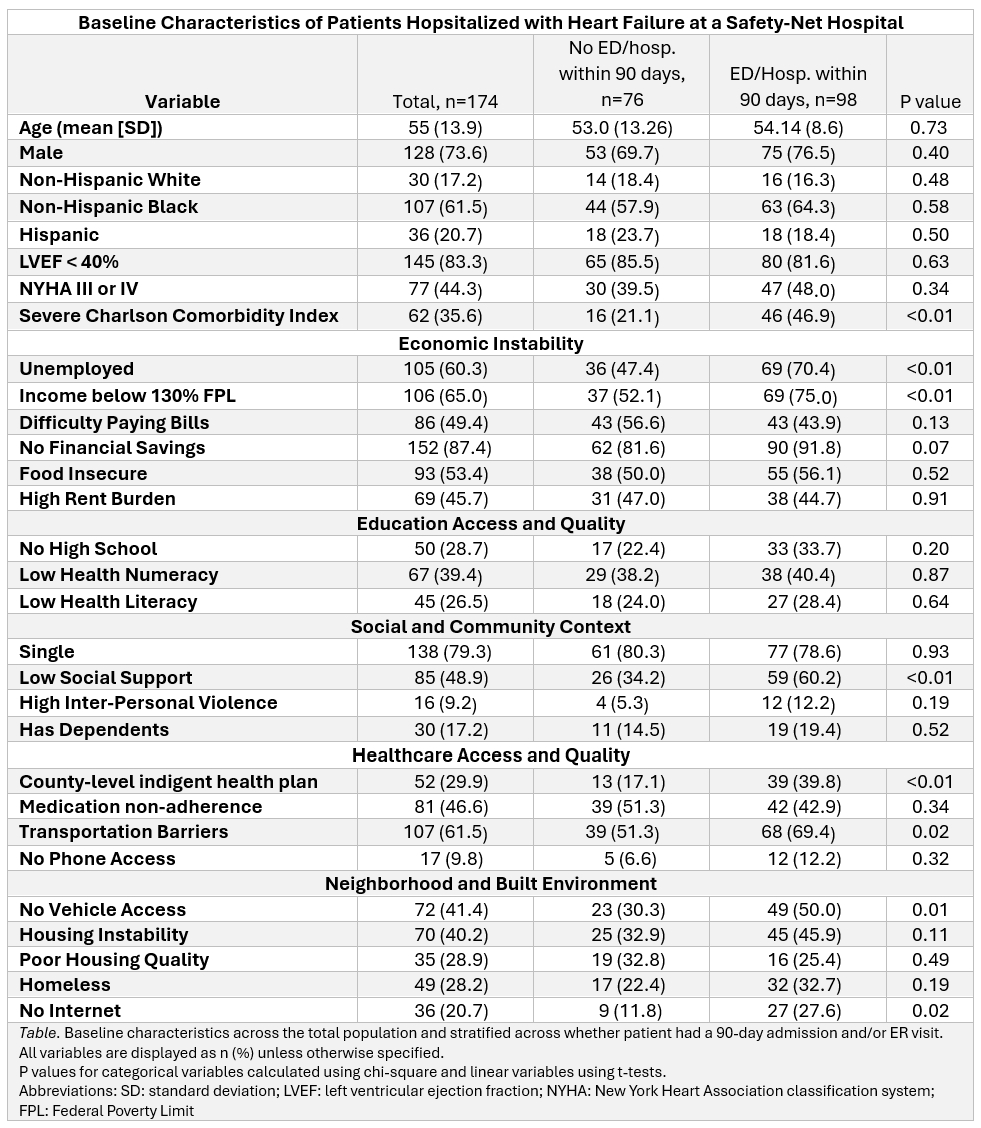
Results: 174 individuals were included (mean age 55 y, 73.6% male, 61.5% Black, 20.7% Hispanic). A high adverse SDOH burden was noted, with 60% of patients unemployed, 65% living below 130% of the federal poverty limit, 53% with food insecurity, 49% with low social support, and 40% with housing instability (28% homeless). In multivariate logistic regression (area under the curve (AUC) = 0.80, F1 score = 0.71), increasing comorbidity burden (aOR 4.84, 95% CI 2.04-12.5, p<0.01), being uninsured (aOR 3.57, 95% CI 1.59-8.50, p<0.01), having low social support (aOR 3.06, 95% CI 1.48-6.53, p<0.01), and having dependents (aOR 2.98, 95% CI 1.13-8.38, p=0.03) were associated with increased odds of 90-day readmission or ER visit (see Table). Conversely, being employed (aOR 0.22, 95% CI 0.09 – 0.52, p<0.01) and having difficulty paying bills (aOR 0.43, 95% CI 0.20-0.88, p=0.02) were associated with decreased odds of 90-day readmission or ER visit.
Conclusions: Hospitalized patients with HF at a safety-net hospital have a high burden of adverse SDOH. Adjusted analysis revealed significant associations of SDOH parameters with 90-day readmission or ER visits, highlighting the need for targeted interventions to recognize and improve adverse SDOH.
Methods: We conducted a prospective, cross-sectional study to identify the prevalence of adverse SDOH among patients hospitalized with acute HF at an urban, safety-net hospital. English or Spanish-speaking patients hospitalized for HF were enrolled between 11/2022-6/2023. We collected data across 5 SDOH domains based on the Healthy People 2030 SDOH Model from the U.S. Department of Health and Human Services. The overall burden of adverse SDOH parameters and their association with hospitalization or emergency room (ER) visits at 90 days was assessed. Multivariate logistic regression models adjusted for selected covariates from the total pool of demographic, clinical, and social covariates using stepwise regression.
Results: 174 individuals were included (mean age 55 y, 73.6% male, 61.5% Black, 20.7% Hispanic). A high adverse SDOH burden was noted, with 60% of patients unemployed, 65% living below 130% of the federal poverty limit, 53% with food insecurity, 49% with low social support, and 40% with housing instability (28% homeless). In multivariate logistic regression (area under the curve (AUC) = 0.80, F1 score = 0.71), increasing comorbidity burden (aOR 4.84, 95% CI 2.04-12.5, p<0.01), being uninsured (aOR 3.57, 95% CI 1.59-8.50, p<0.01), having low social support (aOR 3.06, 95% CI 1.48-6.53, p<0.01), and having dependents (aOR 2.98, 95% CI 1.13-8.38, p=0.03) were associated with increased odds of 90-day readmission or ER visit (see Table). Conversely, being employed (aOR 0.22, 95% CI 0.09 – 0.52, p<0.01) and having difficulty paying bills (aOR 0.43, 95% CI 0.20-0.88, p=0.02) were associated with decreased odds of 90-day readmission or ER visit.
Conclusions: Hospitalized patients with HF at a safety-net hospital have a high burden of adverse SDOH. Adjusted analysis revealed significant associations of SDOH parameters with 90-day readmission or ER visits, highlighting the need for targeted interventions to recognize and improve adverse SDOH.
More abstracts on this topic:
A Bridge from Sweet to Sour: A Case of Recurrent Myocardial Stunning in Diabetic Ketoacidosis
Satish Vikyath, Pargaonkar Sumant, Slipczuk Leandro, Schenone Aldo, Maliha Maisha, Chi Kuan Yu, Sunil Kumar Sriram, Borkowski Pawel, Vyas Rhea, Rodriguez Szaszdi David Jose Javier, Kharawala Amrin, Seo Jiyoung
β1 Adrenergic Receptor Autoantibodies Promote Heart Failure Though Activation of Prostaglandin E2 Receptor EP1/Phosphodiesterase 4B PathwayCao Ning, Qiu Hui, Li Hongwei