Final ID: MDP1655
Contemporary Practice Patterns of Vasoactive Agents in Cardiogenic Shock: An Analysis of the AHA Cardiogenic Shock Registry
Abstract Body (Do not enter title and authors here): Background: Contemporary practice patterns regarding selection of vasoactive agents in cardiogenic shock (CS) have not been well characterized.
Methods: This analysis utilized CS admissions (n=4,311) captured in the American Heart Association (AHA) CS Registry across 64 sites from 2022-2024. Vasoactive agents used within 6h of CS onset were captured in the eCRF, and categorized as inodilators (dobutamine, milrinone), inopressors (norepinephrine, epinephrine, dopamine), or pure vasopressors (vasopressin, phenylephrine). CS etiology was classified as per the Shock Academic Research Consortium definitions: AMI-CS and HF-CS (acute-on-chronic and de novo HF). Subgroup analyses were performed by preceding cardiac arrest status.
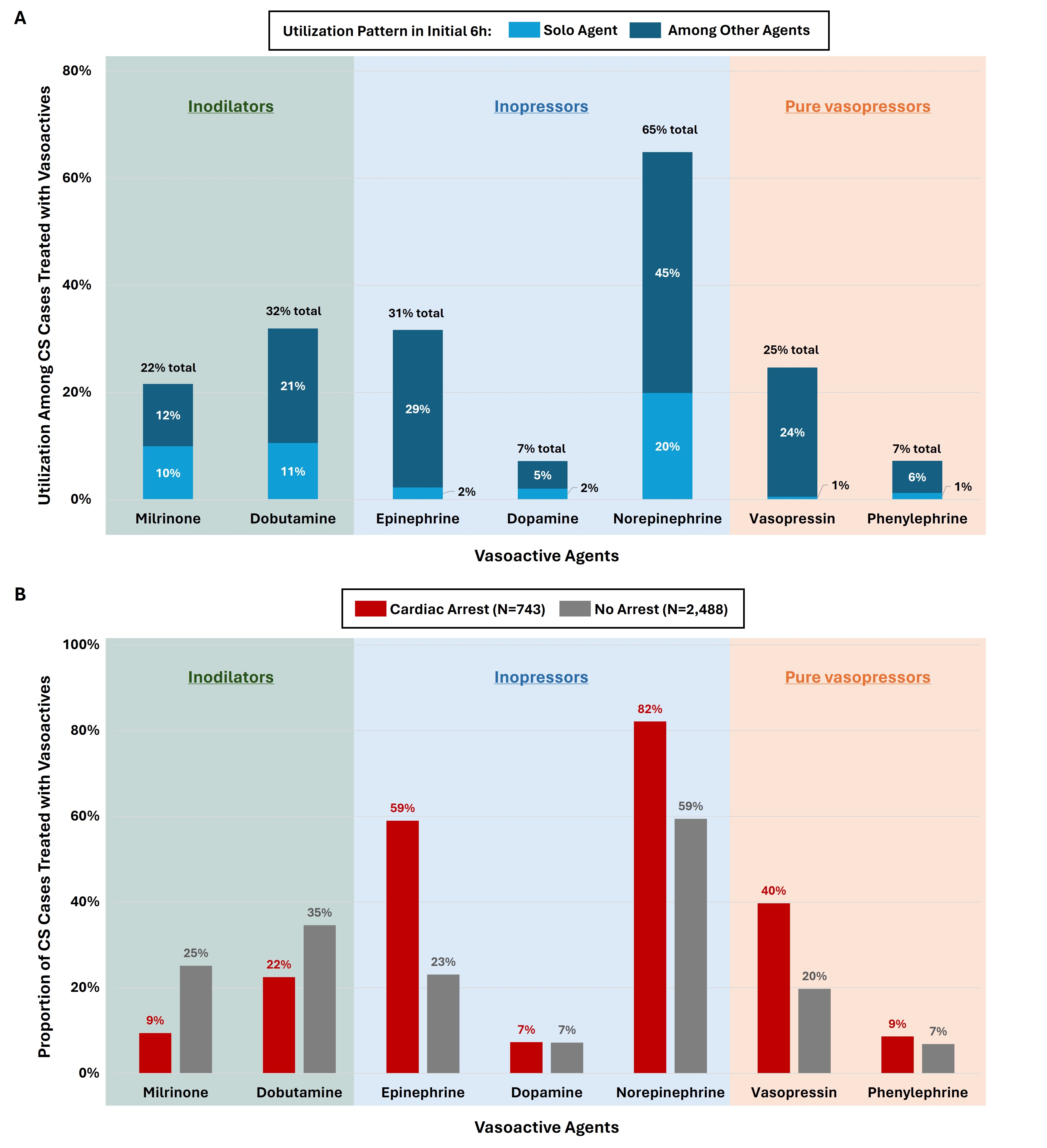
Results: Overall, 3,331 patients (77% of all CS) were treated with ≥1 vasoactive agents in the initial 6h of CS onset (46% with single vs. multiple agents). Inopressors were the most frequently used vasoactive category, with norepinephrine being the most frequently utilized agent (Fig A). Phenylephrine and dopamine were the least frequently employed (Fig A). Stratifying by CS etiology, inodilators were more commonly used for HF-CS vs. AMI-CS (OR [95% CI], 3.05 [2.59-3.59]), driven primarily by those with acute-on-chronic vs. de novo HF (OR 2.95 [2.30-3.78]), as well as in patients with pre-existing pulmonary HTN (OR 2.13 [1.61-2.81]). A total of 743 patients had preceding cardiac arrest; inopressors were more frequently used among those with vs. without preceding cardiac arrest (OR 7.96 [5.84-10.85]; Fig B). Among patients who were treated with ≥2 agents in the initial 6h (n=1,788), the most common two-agent combinations were norepinephrine with epinephrine (45%), norepinephrine with vasopressin (40%) and norepinephrine with dobutamine (30%).
Conclusions: Norepinephrine is the most commonly utilized vasoactive agent (~2/3) in a broad population presenting with CS in contemporary practice, with epinephrine being used in ~1/3. However, CS etiology and illness severity are associated with differential practice patterns for vasoactive selection. These data provide the first snapshot of the landscape of contemporary vasoactive therapy in the US in the AHA CS Registry.
Methods: This analysis utilized CS admissions (n=4,311) captured in the American Heart Association (AHA) CS Registry across 64 sites from 2022-2024. Vasoactive agents used within 6h of CS onset were captured in the eCRF, and categorized as inodilators (dobutamine, milrinone), inopressors (norepinephrine, epinephrine, dopamine), or pure vasopressors (vasopressin, phenylephrine). CS etiology was classified as per the Shock Academic Research Consortium definitions: AMI-CS and HF-CS (acute-on-chronic and de novo HF). Subgroup analyses were performed by preceding cardiac arrest status.
Results: Overall, 3,331 patients (77% of all CS) were treated with ≥1 vasoactive agents in the initial 6h of CS onset (46% with single vs. multiple agents). Inopressors were the most frequently used vasoactive category, with norepinephrine being the most frequently utilized agent (Fig A). Phenylephrine and dopamine were the least frequently employed (Fig A). Stratifying by CS etiology, inodilators were more commonly used for HF-CS vs. AMI-CS (OR [95% CI], 3.05 [2.59-3.59]), driven primarily by those with acute-on-chronic vs. de novo HF (OR 2.95 [2.30-3.78]), as well as in patients with pre-existing pulmonary HTN (OR 2.13 [1.61-2.81]). A total of 743 patients had preceding cardiac arrest; inopressors were more frequently used among those with vs. without preceding cardiac arrest (OR 7.96 [5.84-10.85]; Fig B). Among patients who were treated with ≥2 agents in the initial 6h (n=1,788), the most common two-agent combinations were norepinephrine with epinephrine (45%), norepinephrine with vasopressin (40%) and norepinephrine with dobutamine (30%).
Conclusions: Norepinephrine is the most commonly utilized vasoactive agent (~2/3) in a broad population presenting with CS in contemporary practice, with epinephrine being used in ~1/3. However, CS etiology and illness severity are associated with differential practice patterns for vasoactive selection. These data provide the first snapshot of the landscape of contemporary vasoactive therapy in the US in the AHA CS Registry.
More abstracts on this topic:
Variation in Vasoactive Treatments for Cardiogenic Shock: Insights from the Critical Care Cardiology Trials Network
Hamilton David, Thompson Andrea, Shriver Jackson, Park Jeong-gun, Michos Zoe, Ketcham Scott, Adie Sarah, Mathis Michael, Patel Siddharth, Morrow David
Cardiac Index At The Time Of Pulmonary Artery Pressure Monitor Implantation And Inotrope Requirement Within 1 YearSiddique Talha, Mitchell Ashley, Panza Gregory, Jaiswal Abhishek, Scatola Andrew