Final ID: MDP1665
Characterization of Isolated Right Ventricular Congestion in Cardiogenic Shock
Abstract Body (Do not enter title and authors here): Introduction: Right ventricular (RV) congestion has been associated with poor outcomes in cardiogenic shock (CS); however, the clinical profile of pts with CS & isolated RV congestion has been less well characterized. We aimed to describe the severity of illness, resource utilization & mortality in pts with isolated RV congestion compared to other congestive profiles.
Methods: The Critical Care Cardiology Trials Network is a multicenter registry of CICUs coordinated by the TIMI Study Group (Boston, MA). Pts with CS with invasive hemodynamic assessment within 24h of CICU admission (2018-2023) & not on mechanical circulatory support (MCS) at the time were included. Congestive profiles were defined by right atrial pressure (RAP) & pulmonary capillary wedge pressure (PCWP): isolated RV (RAP≥12 & PCWP<18); isolated left ventricular (LV: RAP<12 & PCWP≥18); biventricular (BiV: RAP≥12 & PCWP≥18), and non-congested (NC: RAP<12 & PCWP<18).
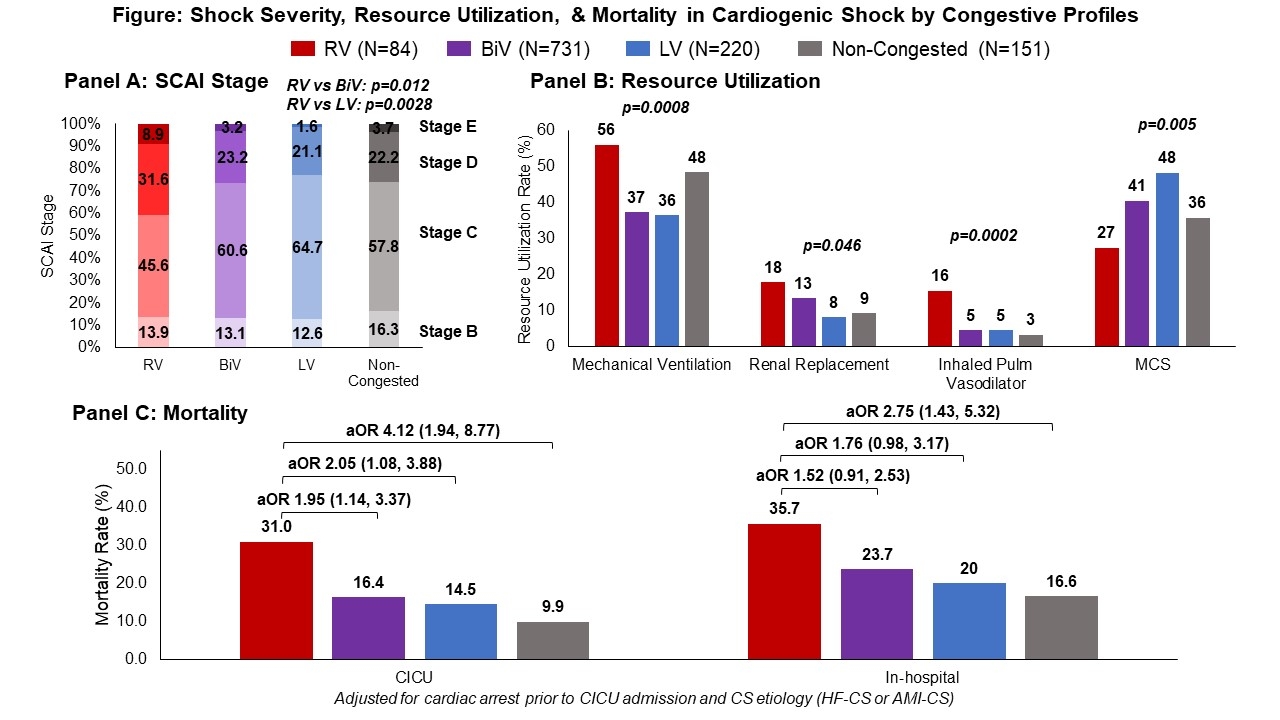
Results: Of 2121 pts with CS, 1186 (56%) met the inclusion criteria with 7.1% classified as RV congestion, 61.6% as BiV, 18.5% as LV & 12.7% as NC. The RV group was more likely to be female & have pulmonary disease than others & less likely to have prior HF or severe valve disease than LV & BiV. The RV congestion group had lower pulmonary artery pulsatility index & higher pulmonary vascular resistance than LV & NC (p<0.05 for all); MAP & CI were similar across groups. PE was a contributor to CS in 1.2% and pHTN in 13.1% of RV cases. The RV group more often presented with de novo HF-CS, where BiV & LV more often had acute on chronic HF-CS. The RV group tended to have worse shock severity by SOFA score, lactate, vasoactive-inotropic score (global p<0.05 for all) & SCAI stage (panel A) and was more likely to have a cardiac arrest (p=0.010). The RV group had greater use of mechanical ventilation & renal replacement, but lower use of MCS (panel B). CICU mortality was significantly higher in the RV group compared to other profiles (panel C), including after adjustment for cardiac arrest & CS etiology.
Conclusion: In pts with CS, isolated RV congestion was associated with the highest presenting illness severity, resource utilization & mortality when compared to other congestive profiles.
Methods: The Critical Care Cardiology Trials Network is a multicenter registry of CICUs coordinated by the TIMI Study Group (Boston, MA). Pts with CS with invasive hemodynamic assessment within 24h of CICU admission (2018-2023) & not on mechanical circulatory support (MCS) at the time were included. Congestive profiles were defined by right atrial pressure (RAP) & pulmonary capillary wedge pressure (PCWP): isolated RV (RAP≥12 & PCWP<18); isolated left ventricular (LV: RAP<12 & PCWP≥18); biventricular (BiV: RAP≥12 & PCWP≥18), and non-congested (NC: RAP<12 & PCWP<18).
Results: Of 2121 pts with CS, 1186 (56%) met the inclusion criteria with 7.1% classified as RV congestion, 61.6% as BiV, 18.5% as LV & 12.7% as NC. The RV group was more likely to be female & have pulmonary disease than others & less likely to have prior HF or severe valve disease than LV & BiV. The RV congestion group had lower pulmonary artery pulsatility index & higher pulmonary vascular resistance than LV & NC (p<0.05 for all); MAP & CI were similar across groups. PE was a contributor to CS in 1.2% and pHTN in 13.1% of RV cases. The RV group more often presented with de novo HF-CS, where BiV & LV more often had acute on chronic HF-CS. The RV group tended to have worse shock severity by SOFA score, lactate, vasoactive-inotropic score (global p<0.05 for all) & SCAI stage (panel A) and was more likely to have a cardiac arrest (p=0.010). The RV group had greater use of mechanical ventilation & renal replacement, but lower use of MCS (panel B). CICU mortality was significantly higher in the RV group compared to other profiles (panel C), including after adjustment for cardiac arrest & CS etiology.
Conclusion: In pts with CS, isolated RV congestion was associated with the highest presenting illness severity, resource utilization & mortality when compared to other congestive profiles.
More abstracts on this topic:
Association between left ventricular trabecular complexity assessed by Fractal analysis and sarcomere mutation in patients with hypertrophic cardiomyopathy
Yang Shujuan
A Stepwise Approach to Identifying and Assessing the Content Validity of Patient-Reported Outcome (PRO) Measures for Use with Adults with Acute Heart FailureO'connor Meaghan, Loughlin Anita, Waldman Laura, Rucker Sloan, Vaghela Shailja, Kwon Namhee, Sikirica Vanja