Final ID: MDP1453
Ventricular Tachycardia Mortality Trends in Oncology: Where Are We Now?
Abstract Body (Do not enter title and authors here): Background
Advancements in chemotherapeutic modalities lead to improved cancer survival rates. While the cardiotoxicity related to the therapies is increasingly recognized, real-world data on ventricular tachycardia (VT) mortality among them is limited.
Objective
This study sought to determine the longitudinal cardiovascular mortality trends related to ventricular tachycardia in the cancer population.
Methods
We queried the CDC WONDER database among patients ≥ 25 years old from 1999 to 2020. Cardiovascular disease was listed as the main cause of death, while VT and cancer were listed as contributing causes of death. We calculated age-adjusted mortality rates (AAMR) per 1,000,000 individuals. We determined the trends over time by estimating the annual percent change (APC) using the Joinpoint regression program.
Results
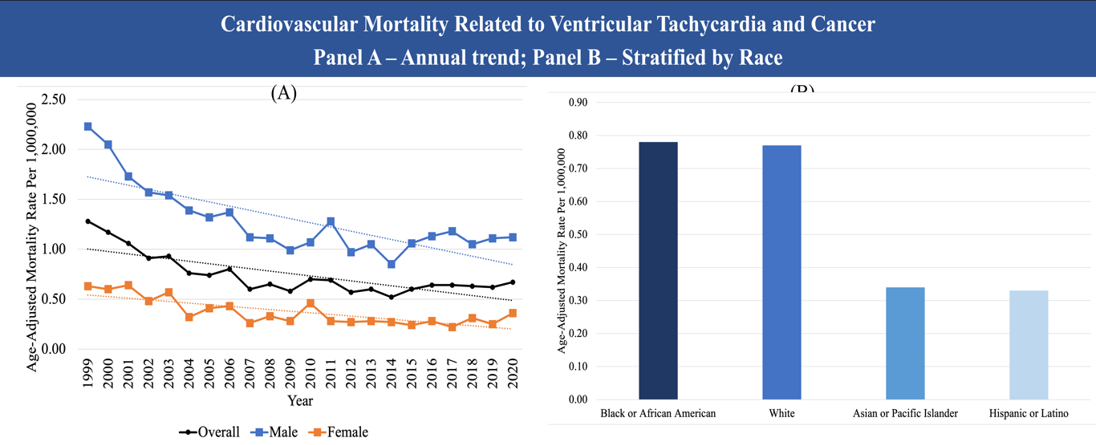
In the study period, there were 3,483 cardiovascular mortalities related to ventricular tachycardia in patients with comorbid cancer. The overall AAMR decreased significantly from 1.28 (95% CI, 1.11-1.44) in 1999 to 0.67 (95% CI, 0.57- 0.77) in 2020, with an average APC of -2.91 (95% CI, -3.95, -1.86). Overall, males had higher AAMR than females (1.25 [95% CI, 1.20 – 1.30] vs. (0.36 [95% CI, 0.34 – 0.39]). African Americans and White patients have comparable AAMR of 0.78 (95% CI, 0.69-0.86) and 0.77 (95% CI, 0.74-0.80), respectively, which were higher than Asians (0.34 [95% CI, 0.25-0.44]) and Hispanics (0.33 [95% CI, 0.27-0.40]). The AAMR was higher in the rural region than in the urban region (0.72 [95% CI, 0.69 – 0.75] vs. 0.76 [95% CI, 0.70 – 0.81]). The West region had the highest AAMR (0.79 [95% CI, 0.74 – 0.85]).
Conclusion
Cardiovascular mortality related to VT in patients with comorbid cancer dropped significantly throughout the years. Further targeted approaches are needed to address the disparities in sex, race, and region.
Advancements in chemotherapeutic modalities lead to improved cancer survival rates. While the cardiotoxicity related to the therapies is increasingly recognized, real-world data on ventricular tachycardia (VT) mortality among them is limited.
Objective
This study sought to determine the longitudinal cardiovascular mortality trends related to ventricular tachycardia in the cancer population.
Methods
We queried the CDC WONDER database among patients ≥ 25 years old from 1999 to 2020. Cardiovascular disease was listed as the main cause of death, while VT and cancer were listed as contributing causes of death. We calculated age-adjusted mortality rates (AAMR) per 1,000,000 individuals. We determined the trends over time by estimating the annual percent change (APC) using the Joinpoint regression program.
Results
In the study period, there were 3,483 cardiovascular mortalities related to ventricular tachycardia in patients with comorbid cancer. The overall AAMR decreased significantly from 1.28 (95% CI, 1.11-1.44) in 1999 to 0.67 (95% CI, 0.57- 0.77) in 2020, with an average APC of -2.91 (95% CI, -3.95, -1.86). Overall, males had higher AAMR than females (1.25 [95% CI, 1.20 – 1.30] vs. (0.36 [95% CI, 0.34 – 0.39]). African Americans and White patients have comparable AAMR of 0.78 (95% CI, 0.69-0.86) and 0.77 (95% CI, 0.74-0.80), respectively, which were higher than Asians (0.34 [95% CI, 0.25-0.44]) and Hispanics (0.33 [95% CI, 0.27-0.40]). The AAMR was higher in the rural region than in the urban region (0.72 [95% CI, 0.69 – 0.75] vs. 0.76 [95% CI, 0.70 – 0.81]). The West region had the highest AAMR (0.79 [95% CI, 0.74 – 0.85]).
Conclusion
Cardiovascular mortality related to VT in patients with comorbid cancer dropped significantly throughout the years. Further targeted approaches are needed to address the disparities in sex, race, and region.
More abstracts on this topic:
A Comparative Study Of Social Determinants, Hypertension, And Life Essential Factors In Alabama And Colorado From The 2021 Behavioral Risk Factor Surveillance System
Chukwunyere Chibuike, Owuor Kevin
All-cause and Cause-specific Mortality Disparities in the District of Columbia: Temporal Trends from 2000 to 2020Hashemian Maryam, Conners Katherine, Powell-wiley Tiffany, Rafi Rebeka, Henriquez Santos Gretell, Shearer Joe, Joo Jungnam, Shiels Meredith, Roger Veronique