Final ID: Mo2093
Impact of Timing of Pacemaker Reimplantation Following Transvenous Lead Removal of Infected Cardiac Implantable Electronic Devices on Hospital Outcomes
Abstract Body (Do not enter title and authors here): Background
The optimal timing of pacemaker reimplantation following transvenous lead removal (TLR) of infected cardiac implantable electronic device (CIED) remains unclear.
Objective
Our study aimed to assess the impact of timing to pacemaker reimplantation after TLR of infected CIED on hospital outcomes.
Method
Using the Nationwide Readmissions Database, patients aged ≥18 years who underwent new pacemaker implantation with percutaneous approach following TLR of infected CIED from 2017 to 2020 were identified. The study population was stratified based on the timing of pacemaker reimplantation following TLR of infected CIED: early (<5 days) vs delayed (≥5 days). Weighted-propensity-score matched conditional multivariable logistic regressions were performed to determine the impact of the timing on various outcomes.
Results
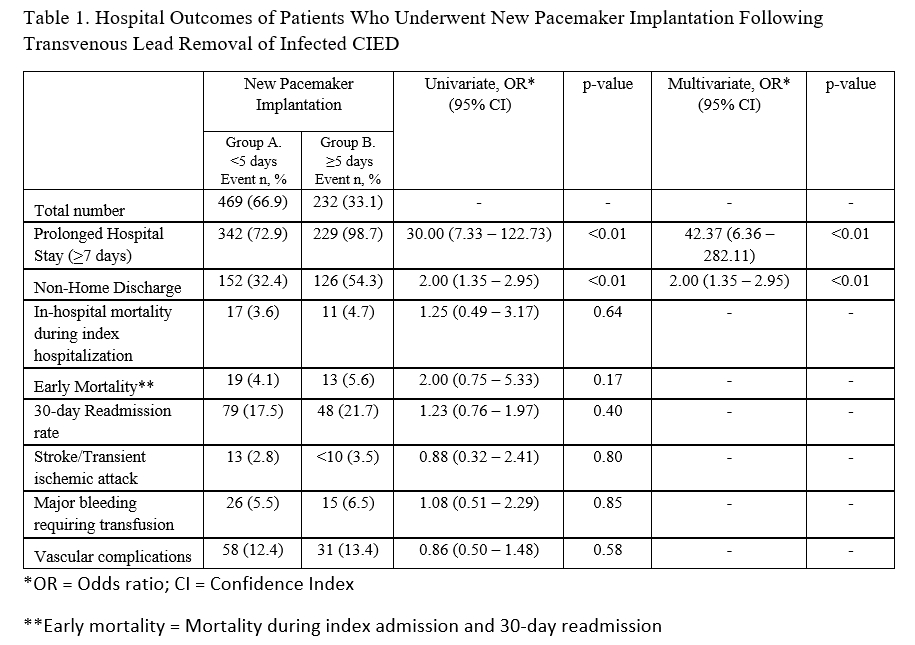
In our study, 469 (66.9%) patients received early device reimplantation, and 232 (33.1%) patients received delayed device reimplantation (≥5 days). Post-procedurally, patients in the delayed group had a higher risk of prolonged hospital stay (95% CI OR: 42.37 (6.36 – 282.11); p<0.01) and non-home discharge (95% CI OR: 2.00 (1.35 – 2.95), p<0.01). There was no significant difference between both groups in the early mortality, 30-day readmission, and procedural complications.
Conclusion
Our study suggests that time-to-device reimplantation from TLR of infected CIED did not affect the overall short-term in-hospital outcomes. However, delayed device reimplantation was associated with a higher rate of prolonged hospital stay and non-home discharge.
The optimal timing of pacemaker reimplantation following transvenous lead removal (TLR) of infected cardiac implantable electronic device (CIED) remains unclear.
Objective
Our study aimed to assess the impact of timing to pacemaker reimplantation after TLR of infected CIED on hospital outcomes.
Method
Using the Nationwide Readmissions Database, patients aged ≥18 years who underwent new pacemaker implantation with percutaneous approach following TLR of infected CIED from 2017 to 2020 were identified. The study population was stratified based on the timing of pacemaker reimplantation following TLR of infected CIED: early (<5 days) vs delayed (≥5 days). Weighted-propensity-score matched conditional multivariable logistic regressions were performed to determine the impact of the timing on various outcomes.
Results
In our study, 469 (66.9%) patients received early device reimplantation, and 232 (33.1%) patients received delayed device reimplantation (≥5 days). Post-procedurally, patients in the delayed group had a higher risk of prolonged hospital stay (95% CI OR: 42.37 (6.36 – 282.11); p<0.01) and non-home discharge (95% CI OR: 2.00 (1.35 – 2.95), p<0.01). There was no significant difference between both groups in the early mortality, 30-day readmission, and procedural complications.
Conclusion
Our study suggests that time-to-device reimplantation from TLR of infected CIED did not affect the overall short-term in-hospital outcomes. However, delayed device reimplantation was associated with a higher rate of prolonged hospital stay and non-home discharge.
More abstracts on this topic:
Circadian Variability in Pediatric Stroke
Lee Sarah, Dlamini Nomazulu, Sreekrishnan Anirudh, Mlynash Michael, Balut Fernanda, Pearson Rachel, Harrar Dana, Surtees Taryn, Mailo Janette, Hassanein Sahar
Comparative Study of Electrophysiologic Pacing Parameters in Patients with Chagas Disease from HondurasBaez Andrew, Chavez Dorys, Tracy Cynthia, Mercader Marco