Final ID: We0088
Mortality Trends in Cerebrovascular Diseases with Underlying Hypertensive or Ischemic Heart Disease in the United States: A CDC-Based Retrospective Analysis (1999–2020)
Abstract Body: Introduction:
Cerebrovascular diseases remain the second leading cause of death globally and the fifth in the United States. The compounding impact of cerebrovascular diseases with hypertensive or ischemic heart disease, along with gender, race, and demographic disparities, remains insufficiently addressed. This study aims to examine mortality trends over two decades (1999-2020) among patients with cerebrovascular disease with coexisting hypertensive or ischemic heart disease.
Methodology:
A retrospective analysis was conducted using the CDC WONDER database (1999–2020) to extract data on cerebrovascular deaths (ICD-10 codes: I60–I69) as the underlying cause, with hypertensive (ICD-10 code: I11) or ischemic heart disease (ICD-10 codes: I20–I25) as contributing causes. Adults aged ≥ 45 years were stratified by gender, race, origin, state, census region, and 2013 urbanization. Age-adjusted mortality rates (AAMRs), standardized to the U.S. 2000 population, and annual percentage changes (APCs) with 95% confidence intervals (CIs) were calculated to assess disparities using Joinpoint Regression.
Results:
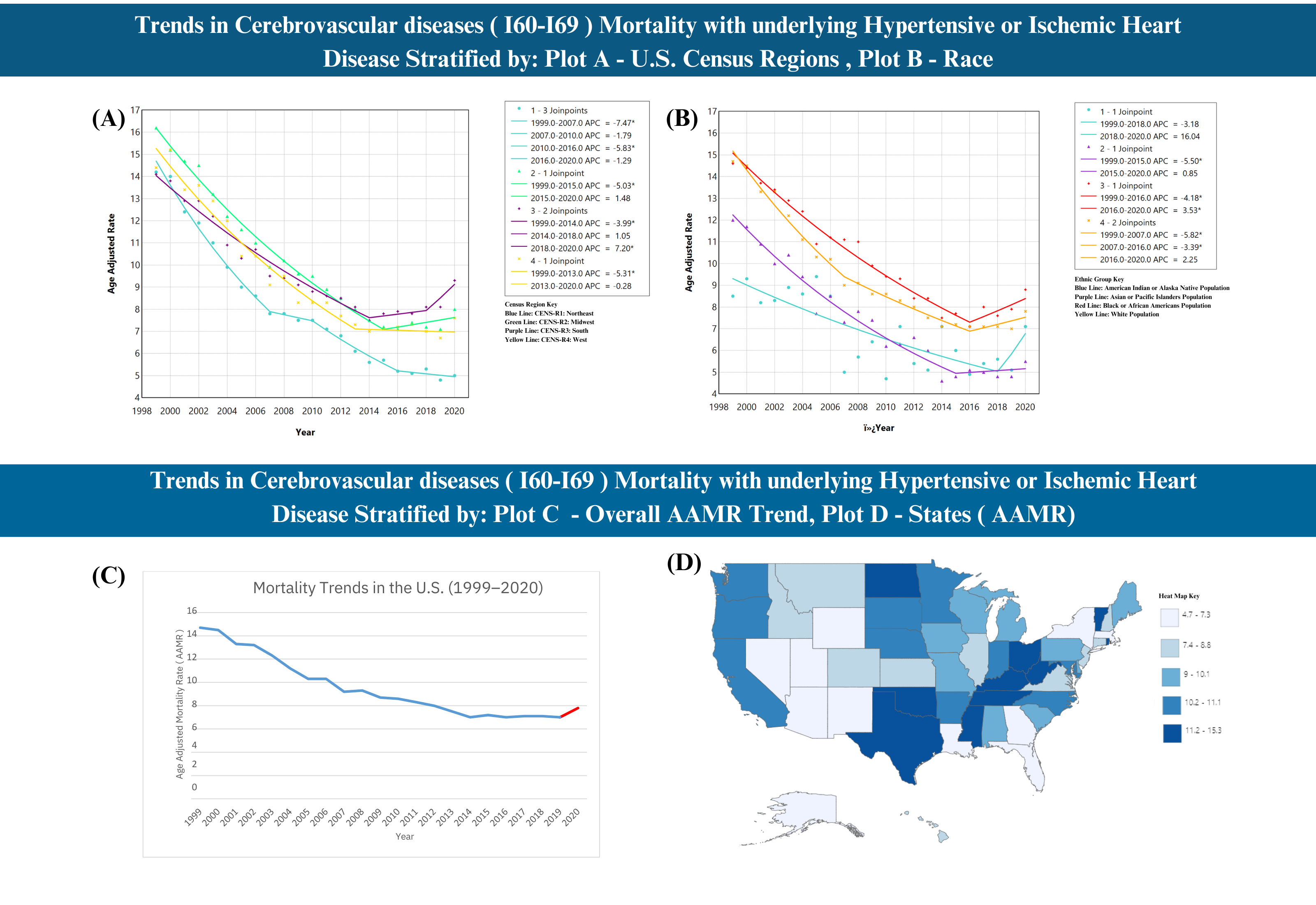
Cerebrovascular diseases with underlying Hypertensive or Ischemic Heart disease in adults aged ≥ 45 years resulted in 239,431 deaths, yielding a mean AAMR of 9.2 (95% CI: 9.2–9.3). AAMRs significantly declined for both genders, with males consistently exhibiting a higher AAMR, with a mean of 11.2 (95% CI: 11.2–11.3). Disparities were evident among males, with Non-Hispanics having an AAMR of 11.4 (95% CI: 11.3–11.5) compared to Hispanics at 8.6 (95% CI: 8.4–8.8).AAMR declined across all racial groups, albeit with an upward inflection among Black or African Americans after 2016 (APC: 3.53, 95% CI: 0.35–10.94, p = 0.033). Similarly, an upward trend also emerged in CENS-R3: South post-2018 (APC: 7.19, 95% CI: 2.14–11.19, p = 0.012). Micropolitan (nonmetro) areas, categorized under the 2013 U.S. Urbanization classification, demonstrated a significant upward inflection from 2018 to 2020, with an APC of 8.78 (95% CI: 1.71–13.24, p = 0.0124). State variations were evident, with Oklahoma exhibiting the highest AAMR at 15.3, while Nevada had the lowest at 4.7.
Conclusion:
Although a period of decline in AAMR was generally observed, significant upward inflections were recently noted in various subgroups, highlighting emerging disparities and regional variations in cerebrovascular disease mortality with underlying hypertensive or ischemic heart disease.
Cerebrovascular diseases remain the second leading cause of death globally and the fifth in the United States. The compounding impact of cerebrovascular diseases with hypertensive or ischemic heart disease, along with gender, race, and demographic disparities, remains insufficiently addressed. This study aims to examine mortality trends over two decades (1999-2020) among patients with cerebrovascular disease with coexisting hypertensive or ischemic heart disease.
Methodology:
A retrospective analysis was conducted using the CDC WONDER database (1999–2020) to extract data on cerebrovascular deaths (ICD-10 codes: I60–I69) as the underlying cause, with hypertensive (ICD-10 code: I11) or ischemic heart disease (ICD-10 codes: I20–I25) as contributing causes. Adults aged ≥ 45 years were stratified by gender, race, origin, state, census region, and 2013 urbanization. Age-adjusted mortality rates (AAMRs), standardized to the U.S. 2000 population, and annual percentage changes (APCs) with 95% confidence intervals (CIs) were calculated to assess disparities using Joinpoint Regression.
Results:
Cerebrovascular diseases with underlying Hypertensive or Ischemic Heart disease in adults aged ≥ 45 years resulted in 239,431 deaths, yielding a mean AAMR of 9.2 (95% CI: 9.2–9.3). AAMRs significantly declined for both genders, with males consistently exhibiting a higher AAMR, with a mean of 11.2 (95% CI: 11.2–11.3). Disparities were evident among males, with Non-Hispanics having an AAMR of 11.4 (95% CI: 11.3–11.5) compared to Hispanics at 8.6 (95% CI: 8.4–8.8).AAMR declined across all racial groups, albeit with an upward inflection among Black or African Americans after 2016 (APC: 3.53, 95% CI: 0.35–10.94, p = 0.033). Similarly, an upward trend also emerged in CENS-R3: South post-2018 (APC: 7.19, 95% CI: 2.14–11.19, p = 0.012). Micropolitan (nonmetro) areas, categorized under the 2013 U.S. Urbanization classification, demonstrated a significant upward inflection from 2018 to 2020, with an APC of 8.78 (95% CI: 1.71–13.24, p = 0.0124). State variations were evident, with Oklahoma exhibiting the highest AAMR at 15.3, while Nevada had the lowest at 4.7.
Conclusion:
Although a period of decline in AAMR was generally observed, significant upward inflections were recently noted in various subgroups, highlighting emerging disparities and regional variations in cerebrovascular disease mortality with underlying hypertensive or ischemic heart disease.
More abstracts on this topic:
A Body Shape Index at Age 25-64 Predicts Mortality and CHD Hospitalization
Shafran Itamar, Krakauer Nir, Krakauer Jesse, Cohen Gali, Gerber Yariv
A Meta-Analysis of Prospective Studies Comparing Short and Longterm Outcomes of Trans-Catheter Aortic Valve Replacement in Patient with and without Cancer:Khan Muhammad Aslam, Haider Adnan, Haider Taimoor, Bhattarai Shraddha, Khan Bilal, Lamichhane Bikal, Shafique Nouman, Rahman Hammad, Aafreen Asna, Muhammad Anza, Bhatia Hitesh, Khan Abid Nawaz Khan, Akbar Usman, Khan Alamzaib