Final ID: We0087
Trends in Intracerebral Hemorrhage Mortality Associated with Essential Hypertension: A 20-Year Analysis Using the CDC WONDER Database (2000–2020)
Abstract Body: Introduction
Intracerebral hemorrhage (ICH) represents a major public health concern, with a mortality rate of over 40% and 20% of survivors remaining functionally independent. While hypertension is the leading cause of ICH, the mortality trends and disparities of ICH in patients with underlying essential hypertension, remain insufficiently explored. This study aims to address these gaps by examining mortality trends in the United States over two decades (2000–2020) using the CDC WONDER database.
Methodology
A retrospective analysis was conducted using the CDC WONDER database (2000 to 2020). The study extracted data for intracerebral hemorrhage (ICD-10 code I61) as the underlying cause of death, with essential hypertension (ICD-10 code 10) as a contributing cause. The analysis included adults aged ≥ 65 years, stratified by gender, race, origin, census region, state, and 2013 urbanization. Age-adjusted mortality rates (AAMRs), standardized to the U.S. 2000 population, and Annual percentage changes (APCs )with 95% Confidence Intervals were calculated to assess disparities using Join Point Regression.
Results
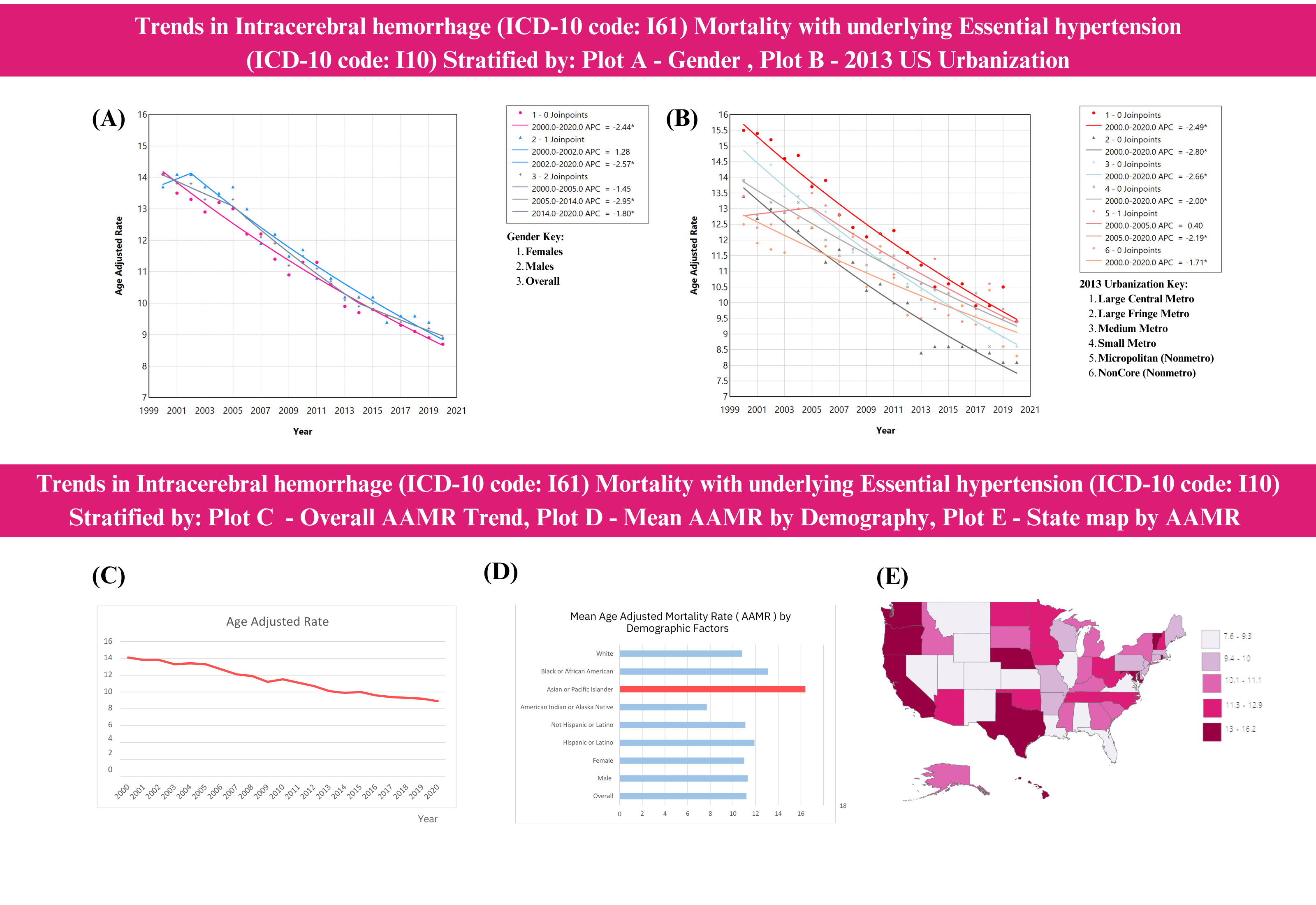
Intracerebral hemorrhage with underlying essential hypertension in adults aged > 65 years caused 98,500 deaths, yielding a mean AAMR of 11.2 (95% CI:11.1–11.2). Overall, the AAMR significantly declined, with an APC of -2.44 (95% CI:-2.73 to -2.20, p < 0.0001). Males consistently had a higher mean AAMR of 11.3 (95% CI:11.1–11.4) than females at 11.0 (95% CI:10.9–11.1). Hispanics had a higher mean AAMR than non-Hispanics, albeit both groups showed a significant decline post-2005 (APC: -2.71 Hispanics, -3.08 non-Hispanics, p < 0.0001). The Asian or Pacific Islander race showed a non-significant upward trend from 2015 to 2020 (APC:1.16, 95% CI: -2.10 to 9.72, p = 0.44), while other races significantly declined. A notable decline was observed in the Northeast (CENS-R1) post-2018 (APC -8.41, 95% CI:-14.84 to -2.46, p < 0.001). Large Central Metro areas, as defined by the US 2013 Urbanization Code, had a higher mean AAMR of 12.1 (95% CI:12.0–12.3) than other regions. State variations were evident, with the District of Columbia (16.2) and California (15.7) having the highest mean AAMRs, while Utah (7.9) and Louisiana (7.6) had the lowest.
Conclusion
Notable regional disparities in AAMR for intracerebral hemorrhage with essential hypertension were identified, with higher rates in large metro areas and specific states, highlighting the need for focused interventions.
Intracerebral hemorrhage (ICH) represents a major public health concern, with a mortality rate of over 40% and 20% of survivors remaining functionally independent. While hypertension is the leading cause of ICH, the mortality trends and disparities of ICH in patients with underlying essential hypertension, remain insufficiently explored. This study aims to address these gaps by examining mortality trends in the United States over two decades (2000–2020) using the CDC WONDER database.
Methodology
A retrospective analysis was conducted using the CDC WONDER database (2000 to 2020). The study extracted data for intracerebral hemorrhage (ICD-10 code I61) as the underlying cause of death, with essential hypertension (ICD-10 code 10) as a contributing cause. The analysis included adults aged ≥ 65 years, stratified by gender, race, origin, census region, state, and 2013 urbanization. Age-adjusted mortality rates (AAMRs), standardized to the U.S. 2000 population, and Annual percentage changes (APCs )with 95% Confidence Intervals were calculated to assess disparities using Join Point Regression.
Results
Intracerebral hemorrhage with underlying essential hypertension in adults aged > 65 years caused 98,500 deaths, yielding a mean AAMR of 11.2 (95% CI:11.1–11.2). Overall, the AAMR significantly declined, with an APC of -2.44 (95% CI:-2.73 to -2.20, p < 0.0001). Males consistently had a higher mean AAMR of 11.3 (95% CI:11.1–11.4) than females at 11.0 (95% CI:10.9–11.1). Hispanics had a higher mean AAMR than non-Hispanics, albeit both groups showed a significant decline post-2005 (APC: -2.71 Hispanics, -3.08 non-Hispanics, p < 0.0001). The Asian or Pacific Islander race showed a non-significant upward trend from 2015 to 2020 (APC:1.16, 95% CI: -2.10 to 9.72, p = 0.44), while other races significantly declined. A notable decline was observed in the Northeast (CENS-R1) post-2018 (APC -8.41, 95% CI:-14.84 to -2.46, p < 0.001). Large Central Metro areas, as defined by the US 2013 Urbanization Code, had a higher mean AAMR of 12.1 (95% CI:12.0–12.3) than other regions. State variations were evident, with the District of Columbia (16.2) and California (15.7) having the highest mean AAMRs, while Utah (7.9) and Louisiana (7.6) had the lowest.
Conclusion
Notable regional disparities in AAMR for intracerebral hemorrhage with essential hypertension were identified, with higher rates in large metro areas and specific states, highlighting the need for focused interventions.
More abstracts on this topic:
Acoramidis Reduces All-Cause Mortality (ACM) and Cardiovascular-Related Hospitalization (CVH): Initial Outcomes From the ATTRibute-CM Open-Label Extension (OLE) Study
Judge Daniel, Masri Ahmad, Obici Laura, Poulsen Steen, Sarswat Nitasha, Shah Keyur, Soman Prem, Cao Xiaofan, Wang Kevin, Pecoraro Maria, Tamby Jean-francois, Gillmore Julian, Katz Leonid, Fox Jonathan, Maurer Mathew, Alexander Kevin, Ambardekar Amrut, Cappelli Francesco, Fontana Marianna, Garcia-pavia Pablo, Grogan Martha, Hanna Mazen
A cerebrovascular longitudinal atlas: different rates of morphological change in aneurysm patients associated with hypertension and diabetesChien Aichi, Salamon Noriko, Vinuela Fernando, Szeder Viktor, Colby Geoffrey, Jahan Reza, Boyle Noel, Villablanca Juan, Duckwiler Gary