Final ID: Su305
Chest Compression Fraction, Bag-mask Ventilation, And Survival From Out-of-hospital Cardiac Arrest: A Multicenter Study
Abstract Body: Background: Ventilation during cardiopulmonary resuscitation (CPR) is poor. Better lung inflation during chest compression pauses is associated with better return of spontaneous circulation (ROSC), survival, and functional neurological survival. Chest compression quality, quantified by chest compression fraction (CCF) >80%, has also served as a guideline target for improved outcomes. We hypothesized that greater chest compression fraction modifies the association between ventilation quality and outcomes.
Methods: We studied patients suffering out-of-hospital cardiac arrest from six sites of the Resuscitation Outcomes Consortium (ROC) Trial of Continuous or Interrupted Chest Compressions during CPR. We performed a subanalysis of patients assigned to the 30:2 CPR arm with ≥ two minutes of thoracic bioimpedance signal recorded with a cardiac defibrillator/monitor. Detectable ventilation waveforms were defined as having a bioimpedance amplitude ≥0.5 Ohm (corresponding to ≥ 250 ml tidal volume) and duration ≥1 sec. We defined a chest compression pause as a break in chest compressions of 3 - 15 sec duration. We dichotomized ventilation into two groups: 1) better lung inflation (≥ one lung inflation waveform in ≥50% of chest compression pauses), and 2) poor lung inflation (waveforms in <50% pauses). We analyzed CCF during bag-mask prior to intubation (if any). We used multivariable logistic regression to assess the relationship among CCF, ventilation, and the outcomes of ROSC, survival, and functional neurologic survival.
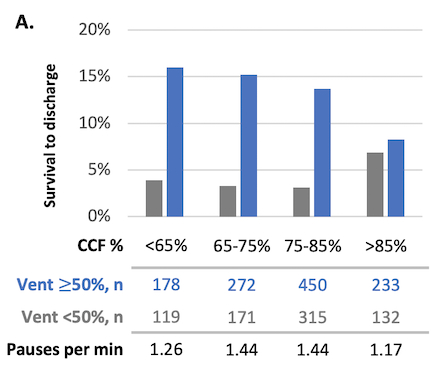
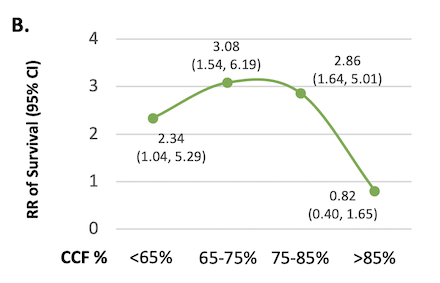
Results: Among 1,976 patients, mean age was 65 years, 66% were male. Most patients received poor ventilation (60%, n=1177) over ventilation over 9.8 ± 4.9 minutes. Median CCF was 0.78 (0.71, 90.84) and 0.78 (0.70, 0.83) for poor and better lung inflation, respectively. For CCF <85%, survival was significantly greater in those who received better ventilation, when compared to poor ventilation, and had greater pauses per minute (Figure A). The beneficial interaction between ventilation and outcome was greater with CCFs of 85% or less, compared to higher CCFs (Figure B). With CCFs >85%, survival did not improve significantly with better ventilation. These results persisted after adjustment for Ustein variables and ROC site.
Conclusions: We observed improved survival with better ventilation until CCF exceeded 85% in the preintubation period, suggesting an optimal strategy with better ventilation and chest compression fractions of 85% or less.
Methods: We studied patients suffering out-of-hospital cardiac arrest from six sites of the Resuscitation Outcomes Consortium (ROC) Trial of Continuous or Interrupted Chest Compressions during CPR. We performed a subanalysis of patients assigned to the 30:2 CPR arm with ≥ two minutes of thoracic bioimpedance signal recorded with a cardiac defibrillator/monitor. Detectable ventilation waveforms were defined as having a bioimpedance amplitude ≥0.5 Ohm (corresponding to ≥ 250 ml tidal volume) and duration ≥1 sec. We defined a chest compression pause as a break in chest compressions of 3 - 15 sec duration. We dichotomized ventilation into two groups: 1) better lung inflation (≥ one lung inflation waveform in ≥50% of chest compression pauses), and 2) poor lung inflation (waveforms in <50% pauses). We analyzed CCF during bag-mask prior to intubation (if any). We used multivariable logistic regression to assess the relationship among CCF, ventilation, and the outcomes of ROSC, survival, and functional neurologic survival.
Results: Among 1,976 patients, mean age was 65 years, 66% were male. Most patients received poor ventilation (60%, n=1177) over ventilation over 9.8 ± 4.9 minutes. Median CCF was 0.78 (0.71, 90.84) and 0.78 (0.70, 0.83) for poor and better lung inflation, respectively. For CCF <85%, survival was significantly greater in those who received better ventilation, when compared to poor ventilation, and had greater pauses per minute (Figure A). The beneficial interaction between ventilation and outcome was greater with CCFs of 85% or less, compared to higher CCFs (Figure B). With CCFs >85%, survival did not improve significantly with better ventilation. These results persisted after adjustment for Ustein variables and ROC site.
Conclusions: We observed improved survival with better ventilation until CCF exceeded 85% in the preintubation period, suggesting an optimal strategy with better ventilation and chest compression fractions of 85% or less.
More abstracts on this topic:
Chest Compression Quality Phenotypes and ROSC in Out-of-Hospital Cardiac Arrest
Raya Krishnamoorthy Banu Priya, Daya Mohamud, Nichol Graham, Stephens Shannon, Carlson Jestin, Panchal Ashish, Wang Henry, Nassal Michelle, Gage Christopher, Kamholz Jacob, Elola Andoni, Aramendi Elisabete, Jaureguibeitia Xabier, Idris Ahamed, Aufderheide Tom
A Multicentre Study for Hands Only CPR (HOCPR) training assessment towards building a ‘Nation of Life Savers” in IndiaRavikumar Thanjavur, Sarma Kvs, Ravikumar Thanjavur, Sarkar Manuj, Debnath Dhrubajyoti, Behera Priyamadhaba, Ghate Jayshri, Trikha Divay, Samantaray A, Madhavi K