Final ID: Su501
Feasibility and Implications of Electrocardiogram-based Prediction of Incessant Refractory Ventricular Fibrillation
Abstract Body: Background
Refractory ventricular fibrillation (R-VF) patients, defined as requiring ≥ 3 shocks during resuscitation of OHCA, have relatively poor outcomes. Prior studies have predicted R-VF using the ECG, suggesting potential to guide early patient-specific treatment for R-VF. However, R-VF comprises multiple phenotypes with distinct defibrillation response profiles: Incessant VF (no shocks terminate VF), recurrent VF (all shocks terminate VF but VF recurs), or mixed VF (shocks variably terminate VF). These phenotypes may have distinct prognoses, and may also respond differently to R-VF treatments such as early antiarrhythmics, modified vasopressor dosing, alternative defibrillation strategies, or expedited invasive interventions. Early prediction of specific R-VF phenotype could potentially improve outcome through preemptive targeting of treatment to individual phenotype.
Aim
We sought to predict incessant R-VF using machine learning analysis of the defibrillator ECG.
Methods
We performed a retrospective study of adult VF OHCA treated by EMS from 2006–2019 in King County WA. We linked a clinical OHCA registry with defibrillator recordings to evaluate ROSC and survival to hospital discharge by VF type (non-refractory; or incessant, recurrent, or mixed R-VF prior to the third shock). To predict incessant R-VF specifically, we used a series of four 2-s ECG segments from each patient within 60s surrounding the first shock. Patients were randomized 65%/35% for training/test. A support vector machine classifier was trained to predict subsequent incessant R-VF using ECG scalograms. Algorithm performance was assessed by area under the receiver operating characteristic curve (AUC) and by sensitivity at >75% specificity.
Results
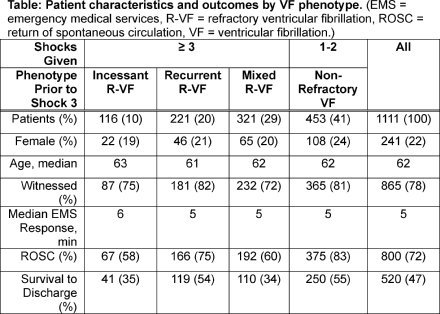
Of 1111 included VF patients, median age was 62, 241 (22%) were female, 658 (59%) were refractory (≥ 3 shocks), 800 (72%) achieved ROSC, and 520 (47%) survived. The incessant R-VF phenotype accounted for 10% (N=116) and had worse ROSC and survival compared to recurrent R-VF and non-refractory patients (Table). Training and test AUCs to predict incessant R-VF were 0.77 (95% CI: 0.72–0.82, N=723) and 0.76 (95% CI: 0.66–0.82, N=388) respectively. Test sensitivity and specificity were 64% and 76%.
Conclusion
Refractory VF comprises distinct phenotypes with disparate outcomes. Incessant R-VF has notably poor prognosis. Machine learning may be able to predict incessant R-VF, potentially guiding preemptive, patient-specific treatments to improve outcome.
Refractory ventricular fibrillation (R-VF) patients, defined as requiring ≥ 3 shocks during resuscitation of OHCA, have relatively poor outcomes. Prior studies have predicted R-VF using the ECG, suggesting potential to guide early patient-specific treatment for R-VF. However, R-VF comprises multiple phenotypes with distinct defibrillation response profiles: Incessant VF (no shocks terminate VF), recurrent VF (all shocks terminate VF but VF recurs), or mixed VF (shocks variably terminate VF). These phenotypes may have distinct prognoses, and may also respond differently to R-VF treatments such as early antiarrhythmics, modified vasopressor dosing, alternative defibrillation strategies, or expedited invasive interventions. Early prediction of specific R-VF phenotype could potentially improve outcome through preemptive targeting of treatment to individual phenotype.
Aim
We sought to predict incessant R-VF using machine learning analysis of the defibrillator ECG.
Methods
We performed a retrospective study of adult VF OHCA treated by EMS from 2006–2019 in King County WA. We linked a clinical OHCA registry with defibrillator recordings to evaluate ROSC and survival to hospital discharge by VF type (non-refractory; or incessant, recurrent, or mixed R-VF prior to the third shock). To predict incessant R-VF specifically, we used a series of four 2-s ECG segments from each patient within 60s surrounding the first shock. Patients were randomized 65%/35% for training/test. A support vector machine classifier was trained to predict subsequent incessant R-VF using ECG scalograms. Algorithm performance was assessed by area under the receiver operating characteristic curve (AUC) and by sensitivity at >75% specificity.
Results
Of 1111 included VF patients, median age was 62, 241 (22%) were female, 658 (59%) were refractory (≥ 3 shocks), 800 (72%) achieved ROSC, and 520 (47%) survived. The incessant R-VF phenotype accounted for 10% (N=116) and had worse ROSC and survival compared to recurrent R-VF and non-refractory patients (Table). Training and test AUCs to predict incessant R-VF were 0.77 (95% CI: 0.72–0.82, N=723) and 0.76 (95% CI: 0.66–0.82, N=388) respectively. Test sensitivity and specificity were 64% and 76%.
Conclusion
Refractory VF comprises distinct phenotypes with disparate outcomes. Incessant R-VF has notably poor prognosis. Machine learning may be able to predict incessant R-VF, potentially guiding preemptive, patient-specific treatments to improve outcome.
More abstracts on this topic:
Deep Learning for Defibrillator Shock Decision Analysis during Manual CPR
Coult Jason, Rea Thomas, Kwok Heemun, King Julia, Bhandari Shiv, Blackwood Jennifer, Johnson Nicholas, Boyle Patrick, Kutz J. Nathan, Kudenchuk Peter
Acceptability and Effectiveness of a Novel, Video-Based CPR and AED Education Program in Canadian SchoolsAllan Katherine, Dhillon Santokh, Mcculloch Holly, Ruether Kim, Zotzman Jeanine, Blanchard Ian, Janczyszyn Mike, Wong Natalie, Oneil Emma, Sapp John