Final ID: Su1002
Association of Post-Arrest Mechanical Ventilation Settings on Survival to Hospital Discharge With Favorable Neurologic Outcome in Children with Cardiac Disease
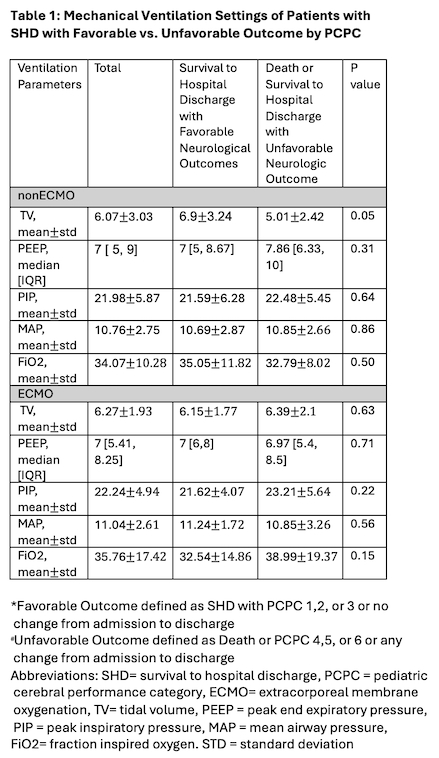
Abstract Body: Introduction: There is a lack of evidence on the optimal mechanical ventilation (MV) settings after pediatric cardiac arrest. The purpose of this study is to investigate the impact of MV settings on survival to hospital discharge (SHD) with favorable neurologic outcome (FNO) in the early post cardiac arrest period. Methods: We conducted a retrospective cohort study of children admitted to a single center pediatric CICU from 9/2016 - 4/2023. We divided our cohort into two groups: patients who did and did not utilize extracorporeal membrane oxygenation (ECMO) during the 48 hours after ROC. We evaluated the association of average values of various MV settings in the 48 hours post-ROSC/ROC: tidal volume (TV, defined as exhaled tidal volume per kg of body weight), peak inspiratory pressure (PIP), peak end expiratory pressure (PEEP), mean airway pressure (MAP), and fraction of inspired oxygen (FiO2) with the association of our primary outcome, SHD with FNO. We defined SHD with FNO as Pediatric Cerebral Performance Category (PCPC) of 1,2, or 3 or no change from admission to discharge. Unfavorable outcome was defined as death or SHD with PCPC of 4,5, or 6. We conducted univariate and multivariate logistic regression analyses, controlling for CPR duration and maximum lactate in the 6 hours post ROSC/ROC. Results: There were 102 index events during the study period. Patients with SHD with FNO compared to those without had lower CPR duration (6.0 [3.0, 18.0] vs. 22.0 [5.0, 43.0] minutes, p=0.0003), incidence of ECPR use (19/57 (33.33%) vs. 24/45 (53.33%), p=0.04), and epinephrine doses used (2.0 [1.0, 6.0] vs. 6.0 [2.0, 8.0], p=0.001). Table 1 shows the MV settings of patients with and without SHD with FNO by PCPC. We found no associations between TV, PIP, PEEP, MAP, and FiO2 with our primary outcome in both ECMO and non-ECMO cohorts. In patients who utilized ECMO, higher TV was associated with lower chances of SHD with FNO. (See Table 2) Conclusions: In this retrospective cohort study of a single center pediatric CICU, early post-arrest TV was associated with SHD with FNO amongst patient supported with ECMO, but not in those who did not utilize ECMO. We did not find an association of PIP, PEEP, MAP, or FiO2 with any outcomes. Future investigations should focus on whether there is a threshold of TV of MV settings that is associated with better outcomes in ECMO patients.
More abstracts on this topic:
Comparison of Right Ventricular Function Changes Between Volume Control and Pressure Support Ventilation Modes: A Prospective Study Using S' Prime Values
Yakkali Shreyas, Agarwal Raksheeth, Kushwaha Ankit, Krishnan Ankita, Anand Dongre Yutika, Adal Bisrat Hussien, Gulani Perminder
Differences in Survival by Resuscitation Response in Pediatric Out-of-Hospital Cardiac Arrest: A Population-Based Study of 900 Children in Houston, TexasStephens Sara, Valdes Santiago, Morris Shaine, Lopez Keila, Lang Anna, Milewicz Dianna, Ostermayer Daniel, Pedroza Claudia, Truong Van Thi Thanh, Chen Bingrui, Wolf Dwayne, Miyake Christina, Persse David, Gumpeni Pramod, Chugh Sumeet, Dezfulian Cameron, Lee Eric, Tran Vinh, Farrier David, Arredondo Sancristobal Maria Jose, Souders Chris, Pierce Michal, Pham Tam Dan