Final ID: Su101
Mesenchymal Stem Cell-Derived Extracellular Vesicles Mitigate Lipopolysaccharide Activation of Porcine Peripheral Blood Mononuclear Cells
Abstract Body: Objective: Systemic inflammation is a well-established component of post-cardiac arrest syndrome (PCAS), a condition responsible for significant morbidity and mortality in patients who achieve return of spontaneous circulation (ROSC) following sudden cardiac arrest. Immune cell activation is pivotal in PCAS pathophysiology and commonly presents ~12hr post-ROSC with endotoxemia (“sterile sepsis”) where lipopolysaccharide (LPS) is present in systemic circulation. Given the paucity of available interventions to inhibit LPS-induced immune activation in the context of PCAS, we investigated the therapeutic potential of mesenchymal stem cell-derived extracellular vesicles (MSC-EVs) to modulate the inflammatory response of porcine peripheral blood mononuclear cells (PBMCs) activated by LPS in vitro.
Methods: Porcine bone marrow-derived MSCs (P2) were cultured for 5 days and serum-starved for 3 days to collect MSC-EVs. These EVs were isolated from conditioned media using size exclusion chromatography and ultracentrifugation, then characterized by nanoparticle tracking analysis (ZetaView) and ExoCheck. Naïve PBMCs from healthy swine were cultured for 1 week before stimulation with either basal media or LPS (5ug/mL). MSC-EVs were added to activated PBMCs (2.5e8–2e9 EVs/well) and inflammatory surface marker expression (flow cytometry), inflammatory cytokine transcripts (qPCR) and release (ELISA), and reactive oxygen/nitrogen species (ROS/RNS) production were assessed 24 hours later.
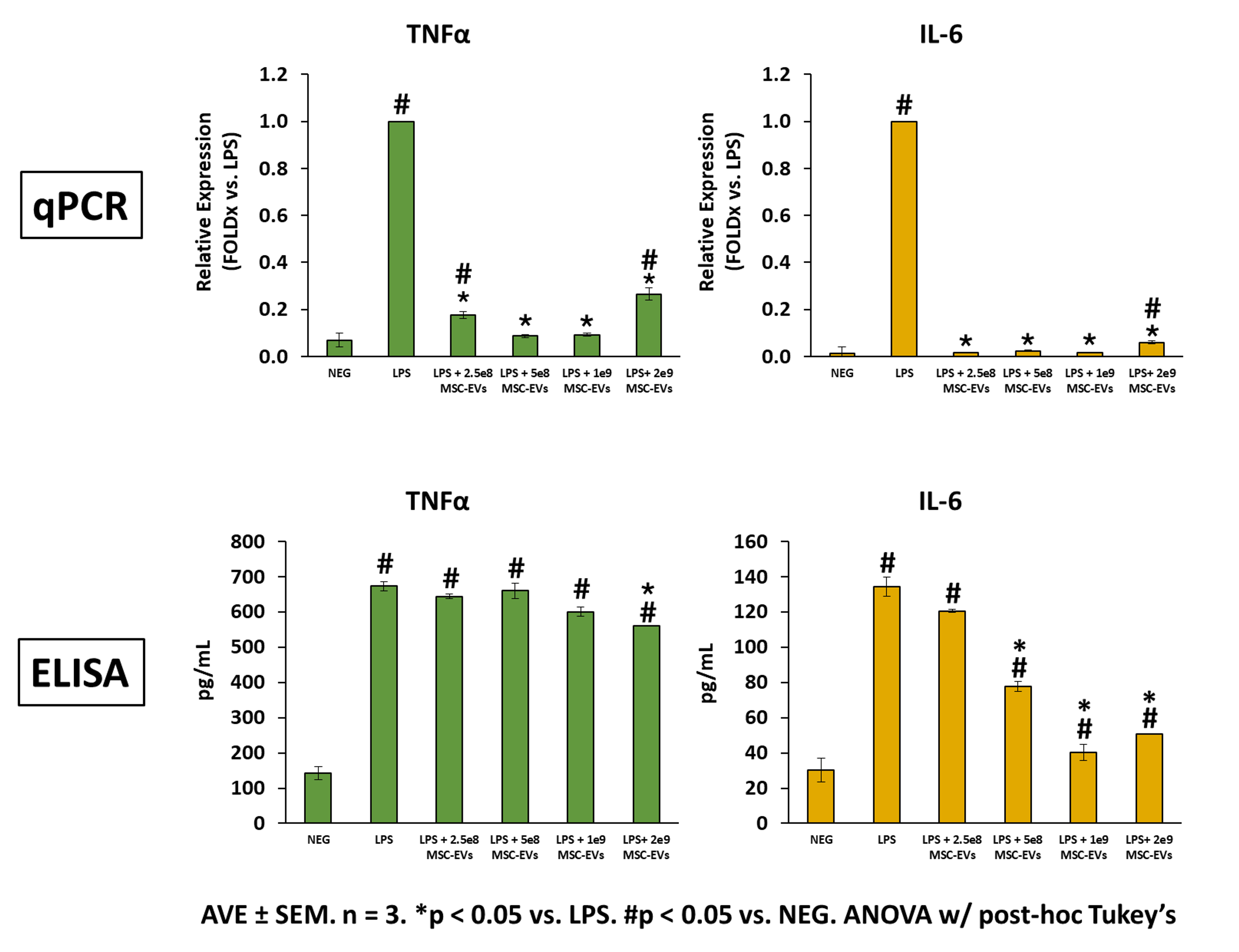
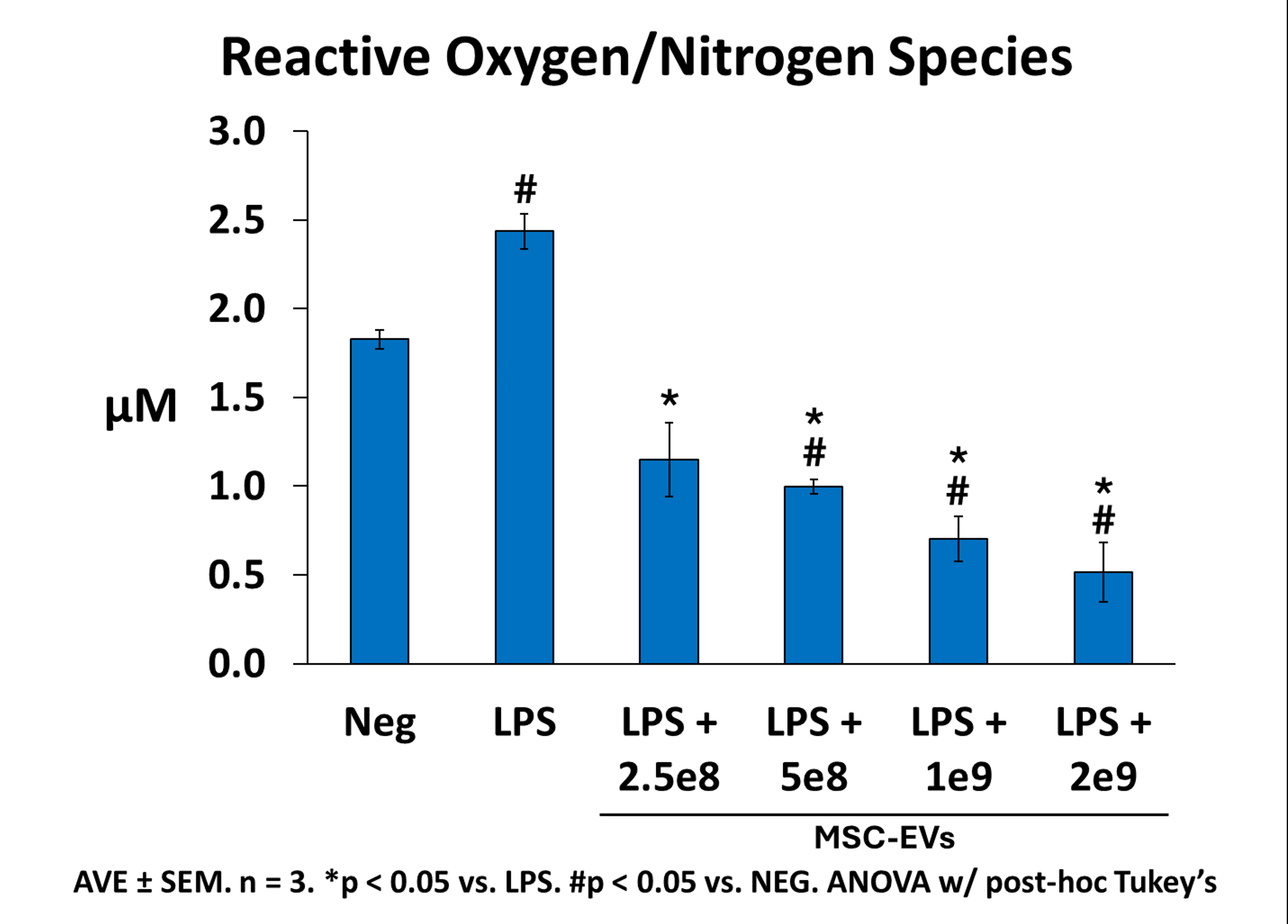
Results: LPS-stimulated PBMC populations exhibited altered surface marker expression consistent with enrichment of inflammatory granulocytes (CD172+CD163-), macrophages (CD14+CD163+), and adhesion molecules (CD172+) compared to basal media (all p<0.05). Addition of MSC-EVs significantly reduced the number of all inflammatory cell populations, with the most prominent effects achieved at the highest EV dose (2e9 EVs/well). Likewise, MSC-EVs significantly attenuated LPS-activated PBMC expression and secretion of TNFα and IL-6 (Figure 1) and decreased ROS/RNS production (Figure 2) in a dose-dependent manner.
Conclusion: MSC-EVs attenuate LPS-induced activation of PBMCs in a dose-dependent manner, as determined by reductions in pro-inflammatory surface marker expression, inflammatory cytokine gene expression and secretion, and ROS/RNS production. These findings indicate that MSC-EVs or MSCs alone, may be a viable therapeutic approach to modulate LPS-mediated immune activation in PCAS.
Methods: Porcine bone marrow-derived MSCs (P2) were cultured for 5 days and serum-starved for 3 days to collect MSC-EVs. These EVs were isolated from conditioned media using size exclusion chromatography and ultracentrifugation, then characterized by nanoparticle tracking analysis (ZetaView) and ExoCheck. Naïve PBMCs from healthy swine were cultured for 1 week before stimulation with either basal media or LPS (5ug/mL). MSC-EVs were added to activated PBMCs (2.5e8–2e9 EVs/well) and inflammatory surface marker expression (flow cytometry), inflammatory cytokine transcripts (qPCR) and release (ELISA), and reactive oxygen/nitrogen species (ROS/RNS) production were assessed 24 hours later.
Results: LPS-stimulated PBMC populations exhibited altered surface marker expression consistent with enrichment of inflammatory granulocytes (CD172+CD163-), macrophages (CD14+CD163+), and adhesion molecules (CD172+) compared to basal media (all p<0.05). Addition of MSC-EVs significantly reduced the number of all inflammatory cell populations, with the most prominent effects achieved at the highest EV dose (2e9 EVs/well). Likewise, MSC-EVs significantly attenuated LPS-activated PBMC expression and secretion of TNFα and IL-6 (Figure 1) and decreased ROS/RNS production (Figure 2) in a dose-dependent manner.
Conclusion: MSC-EVs attenuate LPS-induced activation of PBMCs in a dose-dependent manner, as determined by reductions in pro-inflammatory surface marker expression, inflammatory cytokine gene expression and secretion, and ROS/RNS production. These findings indicate that MSC-EVs or MSCs alone, may be a viable therapeutic approach to modulate LPS-mediated immune activation in PCAS.
More abstracts on this topic:
Clickable Extracellular Vesicles for Localized Abdominal Aortic Aneurysm Repair
Marini Ande, Otto Ellen, Li Bo, Weinbaum Justin, Ren Xi, Campbell Phil, Curci John, Vorp David
A Recalled Experience of Death Among Cardiac Arrest Survivors Is Associated with Improved Psychological OutcomesGoins Imani, Ingram Cambell, Wei Lijing, Gonzales Anelly, He Tun, Moore Sacha, Parnia Sam