Final ID: Or112
Tracheal Intubation During Pediatric In-Hospital Cardiac Arrest: Trends and Association with Survival
Abstract Body: Background:
Pediatric life support guidelines defer recommendation for or against intra-arrest intubation during IHCA. A prior observational study (2000-2014) identified an association of intra-arrest intubation with lower rates of survival to hospital discharge (SHD). Changes in clinical practice (e.g., patient selection, delaying intubation, CPR quality) may have mitigated potential harm.
Aim:
Determine the association between intra-arrest intubation and SHD in a recent cohort of children with IHCA.
Hypothesis:
Intra-arrest intubation is associated with increased odds of SHD.
Methods:
Retrospective cohort study of children with index IHCA without an invasive airway at time of CPR in the Get with the Guidelines registry from 2000-2022. We performed a time-dependent propensity-score matched analysis. Patients intubated in a given minute were matched with patients at-risk of intubation in the same minute based on a propensity score derived from multiple patient, arrest and hospital characteristics, with forced matching on stratification variables (age group, illness category) and replacement of controls. We assessed the association between intra-arrest intubation and SHD using a mixed-effects logistic regression model, with random effects to account for matched data and clustering by hospital, and weighting for the number of times a patient was included as a control.
Results:
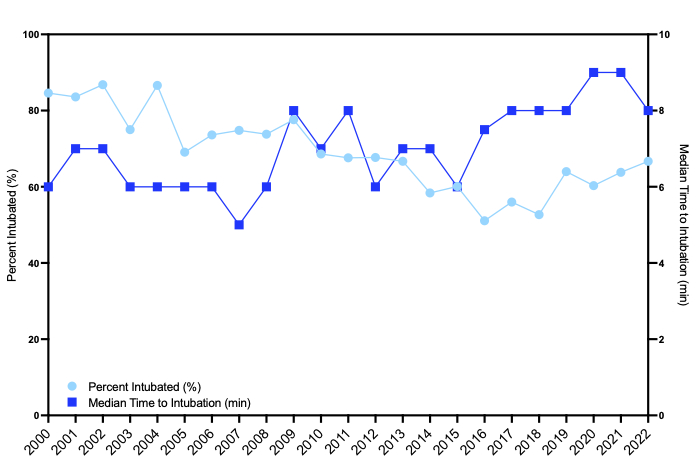
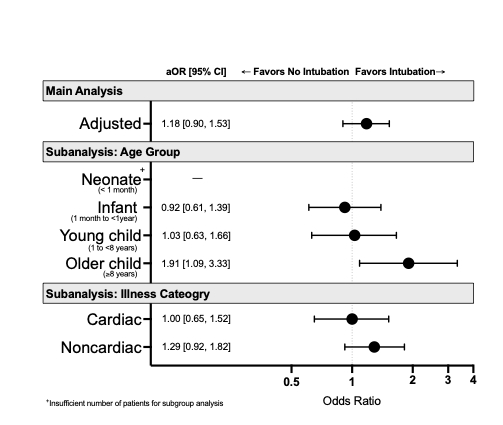
Of 3,262 patients with median age 1 [IQR: 0.3, 8] years, 2,164 (66.3%) were intubated, and 1,748 (53.6%) survived to hospital discharge. Intubation rates decreased from 84.6% to 66.7% across the study period (Figure 1, non-parametric test for trend, p<0.001). Median time to intubation was 7 [4, 12] minutes and increased across the study period (p<0.001). In the recent cohort (2017-2022, n=1192), there was no association between intra-arrest intubation and SHD (aOR 1.18, 95% CI: 0.90, 1.53). In a subgroup analysis of children >8 years, being intubated compared to not being intubated in a given minute was associated with increased odds of SHD (aOR 1.91, 95% CI: 1.09, 3.33) (Figure 2).
Conclusions: In a recent (2017-2022) cohort of children with IHCA, intra-arrest intubation was not associated with increased odds of survival to hospital discharge. In a subgroup of children >8 years, intra-arrest intubation was associated with increased odds of survival. We speculate that secular changes in airway management may partially explain the lack of harm identified in our recent cohort.
Pediatric life support guidelines defer recommendation for or against intra-arrest intubation during IHCA. A prior observational study (2000-2014) identified an association of intra-arrest intubation with lower rates of survival to hospital discharge (SHD). Changes in clinical practice (e.g., patient selection, delaying intubation, CPR quality) may have mitigated potential harm.
Aim:
Determine the association between intra-arrest intubation and SHD in a recent cohort of children with IHCA.
Hypothesis:
Intra-arrest intubation is associated with increased odds of SHD.
Methods:
Retrospective cohort study of children with index IHCA without an invasive airway at time of CPR in the Get with the Guidelines registry from 2000-2022. We performed a time-dependent propensity-score matched analysis. Patients intubated in a given minute were matched with patients at-risk of intubation in the same minute based on a propensity score derived from multiple patient, arrest and hospital characteristics, with forced matching on stratification variables (age group, illness category) and replacement of controls. We assessed the association between intra-arrest intubation and SHD using a mixed-effects logistic regression model, with random effects to account for matched data and clustering by hospital, and weighting for the number of times a patient was included as a control.
Results:
Of 3,262 patients with median age 1 [IQR: 0.3, 8] years, 2,164 (66.3%) were intubated, and 1,748 (53.6%) survived to hospital discharge. Intubation rates decreased from 84.6% to 66.7% across the study period (Figure 1, non-parametric test for trend, p<0.001). Median time to intubation was 7 [4, 12] minutes and increased across the study period (p<0.001). In the recent cohort (2017-2022, n=1192), there was no association between intra-arrest intubation and SHD (aOR 1.18, 95% CI: 0.90, 1.53). In a subgroup analysis of children >8 years, being intubated compared to not being intubated in a given minute was associated with increased odds of SHD (aOR 1.91, 95% CI: 1.09, 3.33) (Figure 2).
Conclusions: In a recent (2017-2022) cohort of children with IHCA, intra-arrest intubation was not associated with increased odds of survival to hospital discharge. In a subgroup of children >8 years, intra-arrest intubation was associated with increased odds of survival. We speculate that secular changes in airway management may partially explain the lack of harm identified in our recent cohort.
More abstracts on this topic:
A Dangerous Right Turn: Primary Right Heart Failure in Mechanically Ventilated Patients—-Prevalence, Inpatient Outcomes, and High Use of Advanced ICU Therapies— A Nationwide Analysis
Khan Dawlat, Chaudhry Hammad, Shehzad Dawood, Riaz Muhammad Faisal, Ahmed Mamoon
Adipocyte-derived small extracellular vesicles and miR-29c-3p promoted apoptosis of cortical neurons in obese mice after resuscitation via downregulating neuronal MCL1Gan Lu, Deng Yalu, Yao Peng, Zhou Tingyuan, Zhou Chao, Cao Yu