Final ID: Sa801
Physiologic Response To Vasopressin Rescue During Pediatric In-Hospital Cardiac Arrest
Hypothesis: Vasopressin is associated with an increase in diastolic blood pressure (DBP) compared to epinephrine in patients with ≥1 dose of epinephrine.
Methods: Single-center retrospective cohort study of pediatric ICU IHCAs with prospectively collected physiologic and arrest event data (2017-2023). Vasopressin subjects received ≥1 dose of epinephrine preceding vasopressin and were matched to patients who received epinephrine at the same time in CPR based on age, illness category (cardiac vs. non-cardiac) and total epinephrine doses prior to the matched dose. DBP response to vasopressor was analyzed with regression discontinuity and the per subject responsiveness (≥5mmHg increase following the dose). A secondary analysis explored time to ROSC from time of vasopressin or epinephrine using Cox regression with censoring of all subjects 20 minutes post-dose.
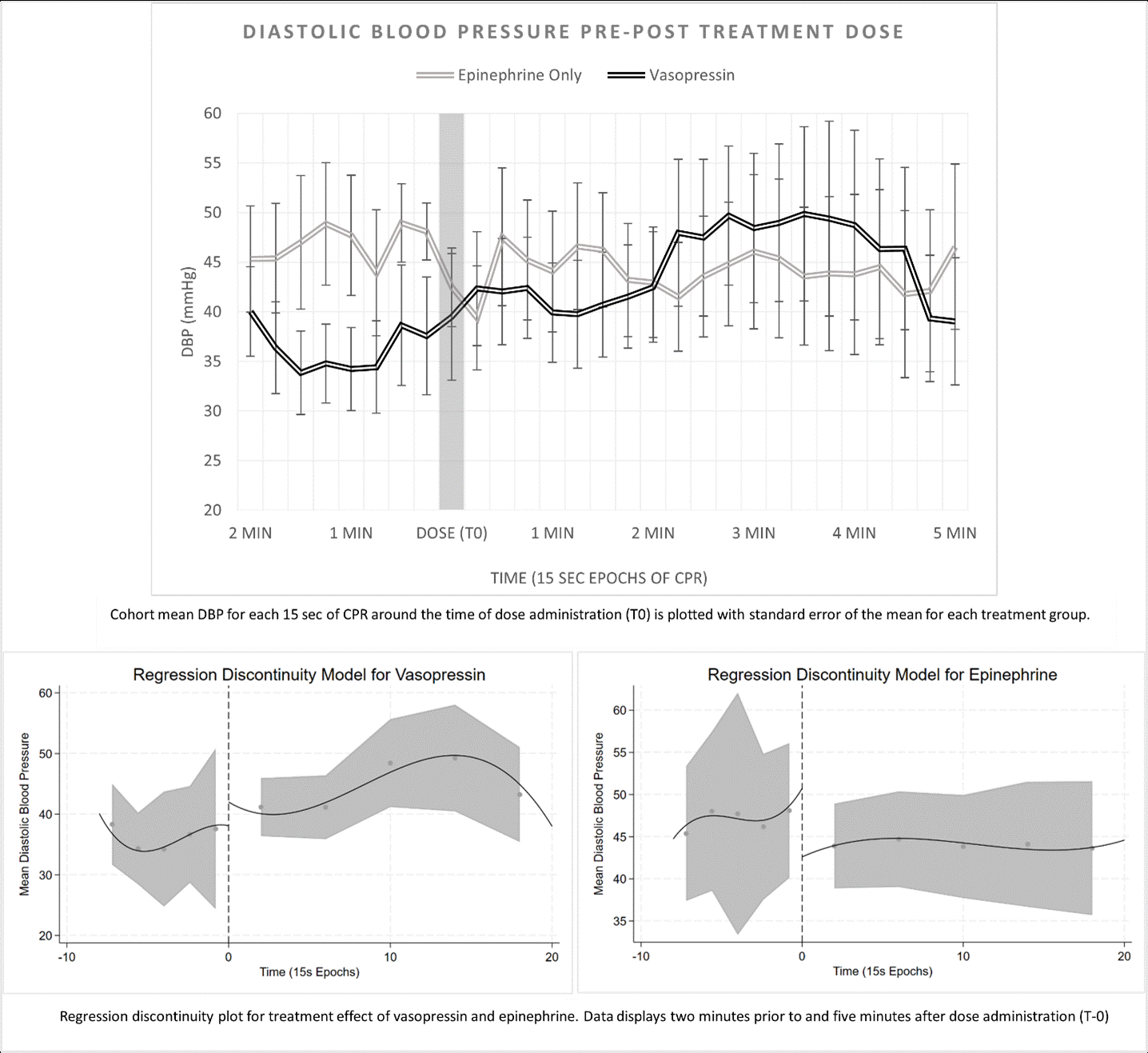
Results: Of 556 IHCAs with ≥1 dose epinephrine, 52 received vasopressin, and 41 met inclusion criteria and matched with epinephrine-only subjects. Median CPR duration was 36.5 [IQR 23, 48] minutes; median time to study dose was 14.5 [10.8, 19] minutes. ROSC occurred in 10/41 (24%) vasopressin subjects and 15/41 (36%) epinephrine subjects (p=0.34). There was no difference in time to ROSC from study dose (aHR 0.73 [95% CI 0.31 -1.7]). Arterial BP waveform data were evaluable in 12/41 (29%) vasopressin and 7/41 (17%) epinephrine subjects. Vasopressor responsiveness occurred in 4/12 (33%) vasopressin and 1/7 (14%) epinephrine subjects (p=0.60). Figure 1 shows trend in DBP by treatment group around drug delivery, along with regression discontinuity plots of DBP for each drug. Regression discontinuity showed a change in DBP of +2.3mmHg after vasopressin (95% CI: –11.4, 16.0) and -5.67mmHg after epinephrine (–15.13, 3.80).
Conclusion: In a small cohort of IHCA patients with ≥1 epinephrine dose, we did not detect a DBP response to vasopressin or epinephrine. Prolonged time to vasopressin in this cohort may have played a role in these findings; a larger sample of children receiving vasopressin earlier in IHCA will be required for future work.
- Loaec, Morgann ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Mehta, Sanjiv ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Kilbaugh, Todd ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Topjian, Alexis ( CHILDRENS HOSPITAL PHILADELPHIA , Wynnewood , Pennsylvania , United States )
- Berg, Robert ( CHILDRENS HOSPITAL OF PHILADELPHIA , Philadelphia , Pennsylvania , United States )
- Nadkarni, Vinay ( CHILDRENS HOSPITAL OF PHILADELPHIA , Philadelphia , Pennsylvania , United States )
- Sutton, Robert ( Childrens Hospital of Philadephia , Philadelphia , Pennsylvania , United States )
- Morgan, Ryan ( Childrens Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Keim, Garrett ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Graham, Kathryn ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Sawhney, Samridhi ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Donoghue, Marion ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Cooper, Kellimarie ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Kienzle, Martha ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- O'halloran, Amanda ( Childrens Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
- Shepard, Lindsay ( Children's Hospital of Philadelphia , Philadelphia , Pennsylvania , United States )
Meeting Info:
Session Info:
ReSS24 Poster Session 108: Pediatrics Intra-Arrest Science
Saturday, 11/16/2024 , 05:15PM - 06:45PM
ReSS24 Poster Session and Reception
More abstracts on this topic:
Jafry Zan, Truong Natalie, Dinh Vi, Joe Yuna
A Comparison of Synchronized Versus Unsynchronized Mechanical Chest Compressions in a Swine ModelMarill Keith, Menegazzi James, Gumucio Jorge, Salcido David
More abstracts from these authors:
Loaec Morgann, Berg Robert, Morgan Ryan, Graham Kathryn, Donoghue Marion, Sawhney Samridhi, Pradhan Anjali, Patterson Elizabeth, Topjian Alexis, Sutton Robert, Reeder Ron
Coronary Perfusion Pressure During Cardiopulmonary Resuscitation is Associated with Event Survival from Pediatric In-hospital Cardiac ArrestKienzle Martha, Sutton Robert, Morgan Ryan, Zuckerberg Jeremy, Patterson Elizabeth, Alvey Jessica, Reeder Ron, Cooper Kellimarie, Graham Kathryn, Nadkarni Vinay, Berg Robert