Final ID: LB48
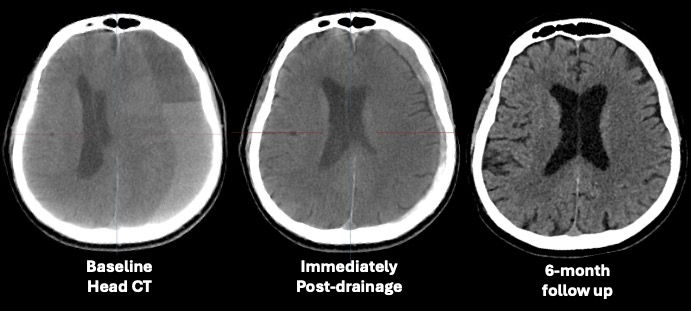
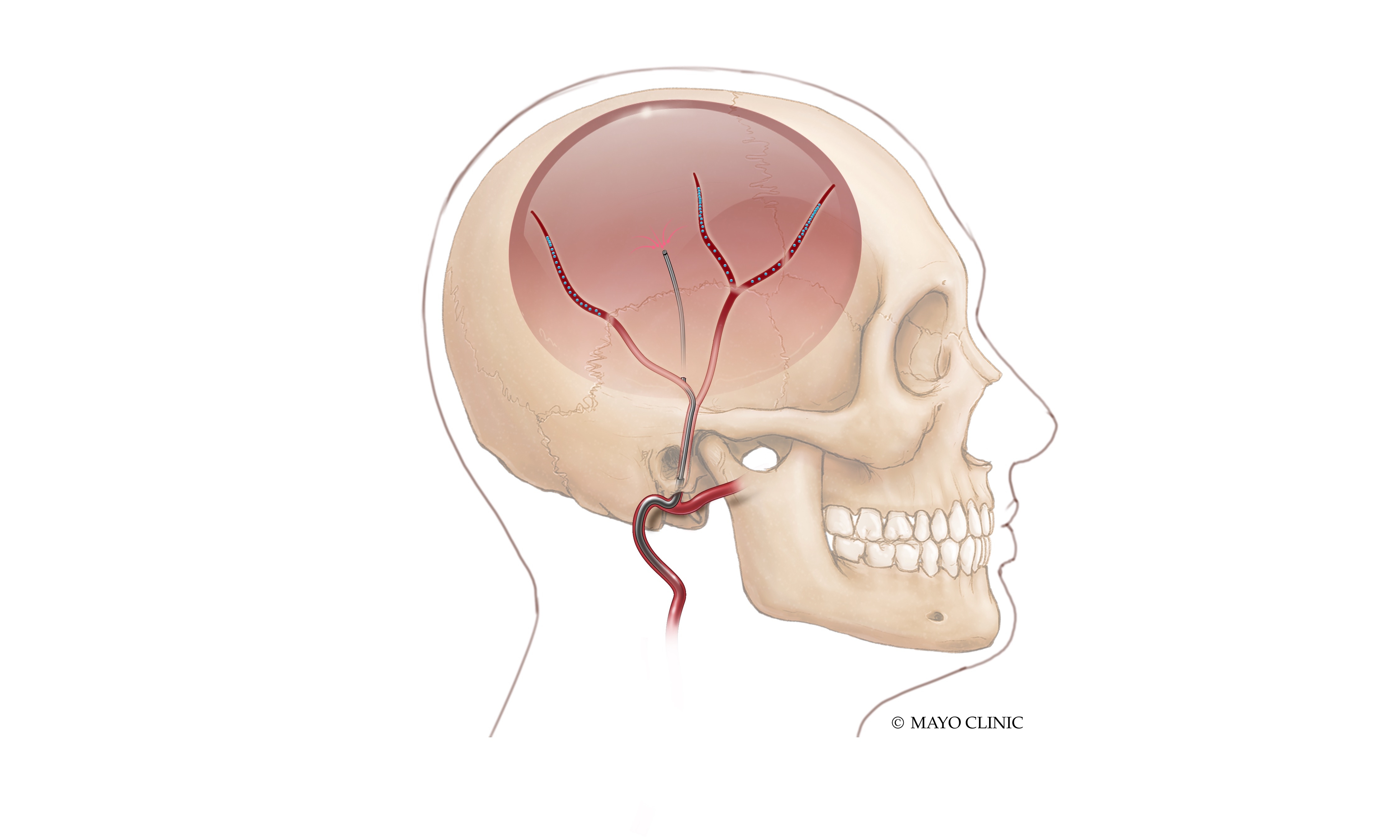
First-in-Human Endovascular Drainage of Non-Acute Subdural-Hematomas and Middle Meningeal Artery Embolization
More abstracts on this topic:
Petautschnig Sigrid, Teo Elliot, Sanders Lauren, Jhamb Ashu, Maingard Julian, Lee Jean, Dixon Barry
A novel methodology for simultaneous analysis of electrical activation parameters and myocardial fibrosis in patients with LBBB and indications to cardiac resynchronization therapyRimskaya Elena, Chmelevsky Mikhail, Aparina Olga, Bazhutina Anastasia, Budanova Margarita, Khamzin Svyatoslav, Stukalova Olga, Ternovoy Sergey, Golitsyn Sergey
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.