Final ID:
Life Threatening Course of Otitis in a Toddler
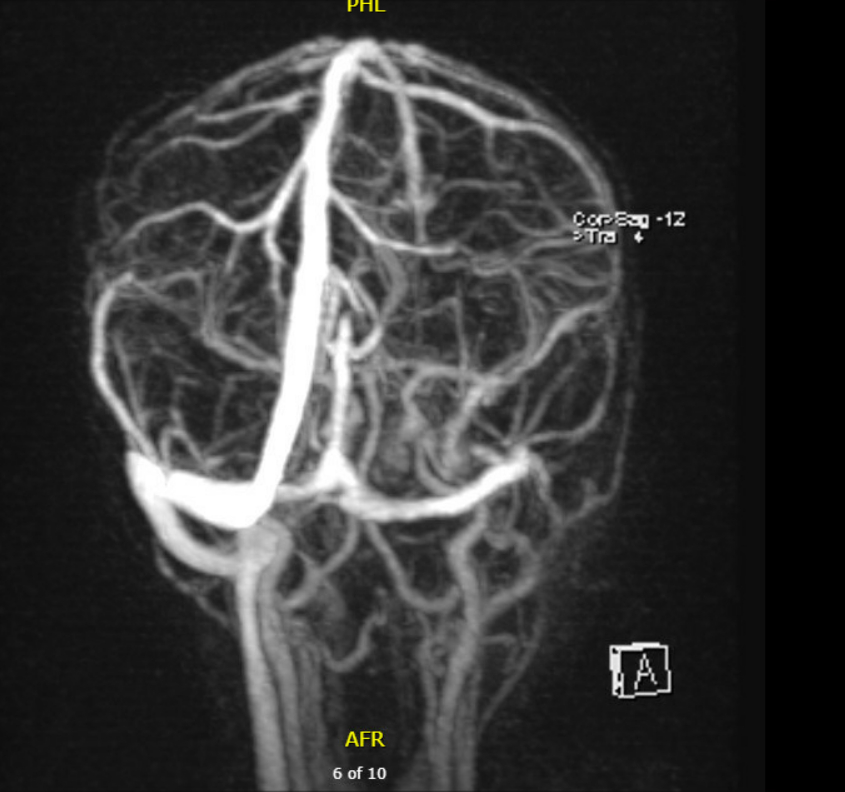
Case Summary: In less than 400 words, please summarize the case. Briefly describe the case and any particular complexities and/or complications encountered.: An unimmunized 18-month-old male presented with two days of fever to 106°F and seven days of foul-smelling left ear drainage. He had recently completed seven days of amoxicillin for left-sided acute otitis media. Initial workup revealed leukocytosis, thrombocytosis, elevated CRP, hyponatremia, and mildly elevated transaminases. A CT brain demonstrated left otitis externa with an adjacent periauricular abscess. Physical examination demonstrated purulent left ear drainage with postauricular swelling and erythema. He was started on empirical ceftriaxone and vancomycin. A CT of the temporal bones confirmed left otitis externa with an adjacent postauricular subperiosteal abscess and mastoiditis. He underwent a mastoidectomy and bilateral tympanostomy tube placement followed by clinical improvement. Five days later, he re-developed fever and had rising inflammatory markers. MRI/MRV brain revealed a cavernous sinus thrombosis extending to the internal jugular vein, consistent with Lemierre’s syndrome (LS). Enoxaparin was initiated for anticoagulation. Anaerobic cultures grew Fusobacterium necrophorum, and antibiotics were adjusted to ampicillin-sulbactam and metronidazole. He improved on 14 days of IV antibiotics followed by 14 days of oral amoxicillin-clavulanate.
Three weeks later, he had complete symptom resolution. MRI showed resolution of the subperiosteal abscess and improved sigmoid sinus and jugular bulb flow with residual chronic thrombus. Given the small size of the remaining thrombus, anticoagulation therapy was discontinued.
LS describes septic thrombophlebitis of the internal jugular vein. It is caused by bacterial invasion through weakened mucosa, most commonly in the setting of pharyngitis and less commonly mastoiditis. Diagnosis is established via contrast-enhanced CT of the neck. Delayed diagnosis worsens prognosis and predisposes to complications such as cavernous sinus thrombosis, septic emboli and stroke. Management requires antibiotics and sometimes surgical intervention or anticoagulation. Associated mortality approaches 18%.
This case illustrates the need for high clinical suspicion and aggressive management of pediatric infections that may evolve into LS. It highlights an unusual association between otitis externa and LS in a toddler with refractory otitis. We emphasize the importance of considering LS in differential of persistent ear infections. Prompt recognition and intervention are critical to preventing life-threatening complications.
Three weeks later, he had complete symptom resolution. MRI showed resolution of the subperiosteal abscess and improved sigmoid sinus and jugular bulb flow with residual chronic thrombus. Given the small size of the remaining thrombus, anticoagulation therapy was discontinued.
LS describes septic thrombophlebitis of the internal jugular vein. It is caused by bacterial invasion through weakened mucosa, most commonly in the setting of pharyngitis and less commonly mastoiditis. Diagnosis is established via contrast-enhanced CT of the neck. Delayed diagnosis worsens prognosis and predisposes to complications such as cavernous sinus thrombosis, septic emboli and stroke. Management requires antibiotics and sometimes surgical intervention or anticoagulation. Associated mortality approaches 18%.
This case illustrates the need for high clinical suspicion and aggressive management of pediatric infections that may evolve into LS. It highlights an unusual association between otitis externa and LS in a toddler with refractory otitis. We emphasize the importance of considering LS in differential of persistent ear infections. Prompt recognition and intervention are critical to preventing life-threatening complications.
More abstracts on this topic:
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)