Final ID:
Recurrent Posterior Circulation Arterial Ischemic Strokes Secondary to Bilateral Vertebral Dissections in a Child
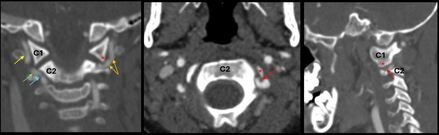
Case Summary: In less than 400 words, please summarize the case. Briefly describe the case and any particular complexities and/or complications encountered.: A 5-year-old boy with no past medical history presented to the emergency department with two weeks of right-sided headaches and fatigue followed by acute onset right-sided weakness and ataxic gait starting 23 hours before arrival. Two months prior, he was hit in the back of the head by a wakeboard at a lake without loss of consciousness or other symptoms. He continued to participate in water sports that day without issue. On the day of presentation, National Institutes of Health Stroke Scale (NIHSS) score was 4 for partial right hemianopia, right facial palsy, right arm drift, and mild dysarthria. Initial head and neck computed tomography (CT) demonstrated infarcts involving bilateral posterior cerebral artery (PCA) territories. There were luminal irregularities of the distal V2 and V3 segments of the left greater than right vertebral arteries (Figure 1), with narrowing of the left vertebral artery below the lateral mass of C1. Anticoagulation with heparin was started on hospital day 2.
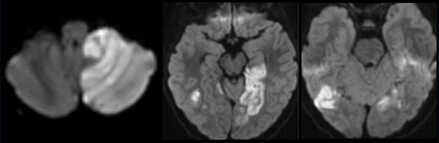
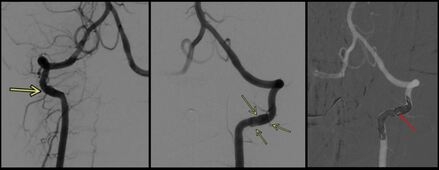
On hospital day 5, he became obtunded and was transferred to the pediatric intensive care unit with a new PCA stroke. He had additional bilateral posterior circulation strokes over the following days with new left posterior inferior cerebellar artery (PICA) occlusion, despite therapeutic heparin (Figure 2). On day 6, digital subtraction angiography (DSA) revealed bilateral vertebral artery dissections. As the left vertebral artery was more severely affected and the source of the left PICA occlusion, the left vertebral artery was sacrificed via transarterial coil embolization (Figure 3). On day 8, he underwent suboccipital decompression for cerebellar edema. On day 13, a DSA showed no compression of the right vertebral artery by neck movements, deeming bow hunter’s syndrome less likely (Figure 3). His previously placed EVD was replaced on day 14 with a ventriculoperitoneal shunt. Aspirin 81 mg was started on day 17. He was discharged on day 24 to inpatient rehabilitation with visual field deficits, bilateral arm weakness, and right-sided dysmetria.
The patient had whole exome sequencing, echocardiogram, and hypercoagulable testing, which did not elucidate an alternative etiology for his strokes. At his 6 month follow up appointment, he was doing well, attending kindergarten, with residual mild dysarthria, visual field deficits, and right-sided dysmetria (despite a left-sided cerebellar infarct), but normal strength and gait. He has had no recurrent strokes since discharge.
On hospital day 5, he became obtunded and was transferred to the pediatric intensive care unit with a new PCA stroke. He had additional bilateral posterior circulation strokes over the following days with new left posterior inferior cerebellar artery (PICA) occlusion, despite therapeutic heparin (Figure 2). On day 6, digital subtraction angiography (DSA) revealed bilateral vertebral artery dissections. As the left vertebral artery was more severely affected and the source of the left PICA occlusion, the left vertebral artery was sacrificed via transarterial coil embolization (Figure 3). On day 8, he underwent suboccipital decompression for cerebellar edema. On day 13, a DSA showed no compression of the right vertebral artery by neck movements, deeming bow hunter’s syndrome less likely (Figure 3). His previously placed EVD was replaced on day 14 with a ventriculoperitoneal shunt. Aspirin 81 mg was started on day 17. He was discharged on day 24 to inpatient rehabilitation with visual field deficits, bilateral arm weakness, and right-sided dysmetria.
The patient had whole exome sequencing, echocardiogram, and hypercoagulable testing, which did not elucidate an alternative etiology for his strokes. At his 6 month follow up appointment, he was doing well, attending kindergarten, with residual mild dysarthria, visual field deficits, and right-sided dysmetria (despite a left-sided cerebellar infarct), but normal strength and gait. He has had no recurrent strokes since discharge.
More abstracts on this topic:
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)