Final ID: WP129
Disparities in the utilization of inpatient rehabilitation facilities for stroke patients in the United States
Abstract Body: Background
We evaluate the contemporary trends and socioeconomic disparities in utilization of post-stroke rehabilitation using statewide inpatient data from 5 states with large and diverse populations.
Methods
We used ICD codes (I60, I61, I63) to identify adult patients (≥18 years) discharged home (including home health), to IRF, or skilled nursing facility (SNF) with acute ischemic stroke (AIS), spontaneous intracerebral hemorrhage (ICH), or subarachnoid hemorrhage (SAH) primary diagnosis from the inpatient databases of Florida, Georgia, Maryland, New York, and Washington (2016-2019). Utilizing multivariable logistic regression multivariable logistic regression with patient-level cluster-robust standard errors, we evaluate the correlates of discharge to IRF (vs. home and SNF) and report the adjusted odds ratios (aOR) and 95% confidence intervals (CI).
Results
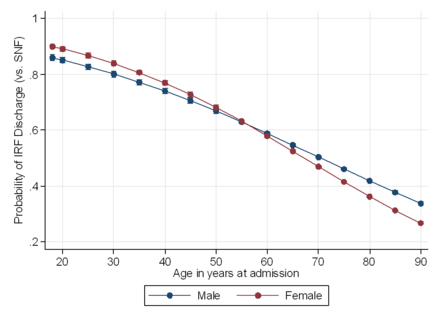
Overall, 335,521 stroke discharges (88.4% AIS, 8.1% ICH, 3.5% SAH) representing 312,316 unique patients (median age [IQR] of 69 [59-80] and 47.9% female) were included. Among these, 21.8% discharges were to IRF, 51.5% to home, and 26.7% to SNF. Between 2016 and 2019, the overall proportion of IRF discharges did not change significantly (21.8% in 2016; 22.1% in 2019). Patients with ICH (vs. AIS) were more likely to be discharged to IRF (vs. home) (aOR, CI: 2.17, 2.10-2.26). Patients discharged to IRF (vs. SNF) were more likely to be privately (vs. Medicare) insured (1.73, 1.66-1.79), and reside in the highest income quartile zip codes, vs. lowest quartile (aOR, CI: 1.31, 1.26-1.35). Conversely, non-Hispanic Black (vs. non-Hispanic White individuals were less likely to be discharged to IRF (vs. SNF) (aOR, CI: 0.92, 0.89 – 0.94). Stroke patients with higher comorbidity burden, as measured by Charlson Comorbidity Index (aOR, CI: 0.88, 0.87-0.89), and those undergoing invasive ventilation (0.79, 0.75-0.83) and tracheostomy (0.35, 0.32-0.38) were also less likely to be discharged to IRF (vs. SNF). We observed an age-dependent association between sex and IRF discharge whereby older females (vs. males) are less likely to be discharged to IRF in lieu of SNF (p-value for interaction <0.001; Figure 1).
Conclusion
Less than 1 in 4 stroke patients receive post-acute IRF care, highlighting a critical gap in achieving optimal stroke recovery. Furthermore, notable sociodemographic disparities persist in IRF utilization. Maximizing pathways for optimal post-stroke recovery remains a critical gap in stroke systems of care.
We evaluate the contemporary trends and socioeconomic disparities in utilization of post-stroke rehabilitation using statewide inpatient data from 5 states with large and diverse populations.
Methods
We used ICD codes (I60, I61, I63) to identify adult patients (≥18 years) discharged home (including home health), to IRF, or skilled nursing facility (SNF) with acute ischemic stroke (AIS), spontaneous intracerebral hemorrhage (ICH), or subarachnoid hemorrhage (SAH) primary diagnosis from the inpatient databases of Florida, Georgia, Maryland, New York, and Washington (2016-2019). Utilizing multivariable logistic regression multivariable logistic regression with patient-level cluster-robust standard errors, we evaluate the correlates of discharge to IRF (vs. home and SNF) and report the adjusted odds ratios (aOR) and 95% confidence intervals (CI).
Results
Overall, 335,521 stroke discharges (88.4% AIS, 8.1% ICH, 3.5% SAH) representing 312,316 unique patients (median age [IQR] of 69 [59-80] and 47.9% female) were included. Among these, 21.8% discharges were to IRF, 51.5% to home, and 26.7% to SNF. Between 2016 and 2019, the overall proportion of IRF discharges did not change significantly (21.8% in 2016; 22.1% in 2019). Patients with ICH (vs. AIS) were more likely to be discharged to IRF (vs. home) (aOR, CI: 2.17, 2.10-2.26). Patients discharged to IRF (vs. SNF) were more likely to be privately (vs. Medicare) insured (1.73, 1.66-1.79), and reside in the highest income quartile zip codes, vs. lowest quartile (aOR, CI: 1.31, 1.26-1.35). Conversely, non-Hispanic Black (vs. non-Hispanic White individuals were less likely to be discharged to IRF (vs. SNF) (aOR, CI: 0.92, 0.89 – 0.94). Stroke patients with higher comorbidity burden, as measured by Charlson Comorbidity Index (aOR, CI: 0.88, 0.87-0.89), and those undergoing invasive ventilation (0.79, 0.75-0.83) and tracheostomy (0.35, 0.32-0.38) were also less likely to be discharged to IRF (vs. SNF). We observed an age-dependent association between sex and IRF discharge whereby older females (vs. males) are less likely to be discharged to IRF in lieu of SNF (p-value for interaction <0.001; Figure 1).
Conclusion
Less than 1 in 4 stroke patients receive post-acute IRF care, highlighting a critical gap in achieving optimal stroke recovery. Furthermore, notable sociodemographic disparities persist in IRF utilization. Maximizing pathways for optimal post-stroke recovery remains a critical gap in stroke systems of care.
More abstracts on this topic:
A ChatGLM-based stroke diagnosis and prediction tool
Song Xiaowei, Wang Jiayi, Ma Weizhi, Wu Jian, Wang Yueming, Gao Ceshu, Wei Chenming, Pi Jingtao
A Fecal-Derived Commensal Bacterium BM109 Reduces Infarct Size and Neurological Deficits in an Ischemic Stroke Rat ModelYoon Chung Eun, Kim You Bin, Nam Hyo Suk
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)