Final ID: WP295
Associations between measures of structural racism and acute ischemic stroke outcomes in the US
Abstract Body: Background: Structural inequity, including structural racism, is increasingly linked to stroke measures. Prior work has shown that ecosocial models quantifying constituent domains of structural racism correlate with acute ischemic stroke (AIS) incidence. It remains unclear if such models can further account for the not yet fully explained racial disparities in stroke outcomes.
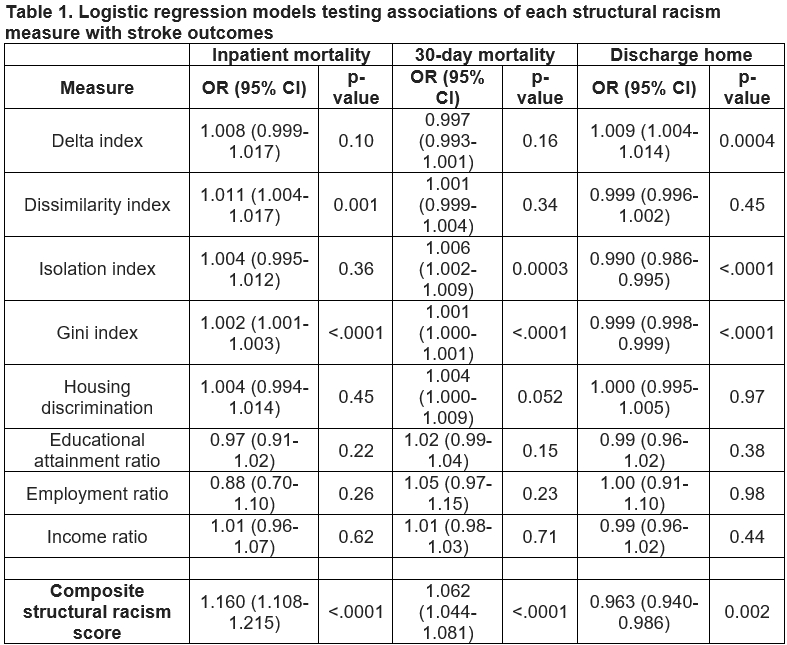
Methods: We performed a national, population-based analysis of Medicare beneficiaries aged >65 years enrolled in Medicare from January 1, 2016 to December 31, 2019, resulting in 71,078,619 eligible adults, of whom 844,406 had a primary diagnosis of AIS. In separate models, we estimated the odds ratio (OR) and 95% confidence intervals (CI) of three outcomes (inpatient mortality, 30-day mortality, and discharge home) using multilevel logistic models for clustered data, with data clustered at the county level. Structural racism variables were tested in separate models, adjusting for sex, age, urban vs. other location, and Black vs. White race.
Results: The composite structural racism score was strongly correlated with inpatient mortality (1.16, 95% CI: 1.10-1.22) without a significant interaction with race (p=0.62). Both 30-day all-cause mortality (p=0.04) and discharge home (p=0.02) significantly interacted with race. For each unit increase in structural racism, Black individuals had 4.5% increased odds of 30-day mortality and 5.8% decreased odds of being discharged home, whereas White patients had a 6.5% increase in 30-day mortality and 3.5% decrease in odds of discharge home.
Conclusions: Both racial and geographic disparities in short-term outcomes after AIS are strongly correlated with structural inequity across the United States.
Methods: We performed a national, population-based analysis of Medicare beneficiaries aged >65 years enrolled in Medicare from January 1, 2016 to December 31, 2019, resulting in 71,078,619 eligible adults, of whom 844,406 had a primary diagnosis of AIS. In separate models, we estimated the odds ratio (OR) and 95% confidence intervals (CI) of three outcomes (inpatient mortality, 30-day mortality, and discharge home) using multilevel logistic models for clustered data, with data clustered at the county level. Structural racism variables were tested in separate models, adjusting for sex, age, urban vs. other location, and Black vs. White race.
Results: The composite structural racism score was strongly correlated with inpatient mortality (1.16, 95% CI: 1.10-1.22) without a significant interaction with race (p=0.62). Both 30-day all-cause mortality (p=0.04) and discharge home (p=0.02) significantly interacted with race. For each unit increase in structural racism, Black individuals had 4.5% increased odds of 30-day mortality and 5.8% decreased odds of being discharged home, whereas White patients had a 6.5% increase in 30-day mortality and 3.5% decrease in odds of discharge home.
Conclusions: Both racial and geographic disparities in short-term outcomes after AIS are strongly correlated with structural inequity across the United States.
More abstracts on this topic:
A Comparative Analysis of Social Demographic and Clinical Factors for Screening for Peripheral Artery Disease in Adult Patients from Primary Care Clinics
Lane Rashon, Jackson Pasha, Anokwuru Ferdinand, Dillard Naomi, Nerlekar Ridhima
Ablation vs. Antiarrhythmic Drugs in Atrial Fibrillation: Real-World Treatment Gaps, Outcomes, and Equity ChallengesRauf Saman, Iqbal Fatima, Bhatti Shehzeen Dua, Masood Natasha, Qureshi Muhammad Maaz, Nawaz Muhammad Hassan
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)