Final ID: TP291
COVID-19 Infection is Associated with Stroke Subtype, Severity, and Outcomes in Patients with Acute Ischemic Stroke
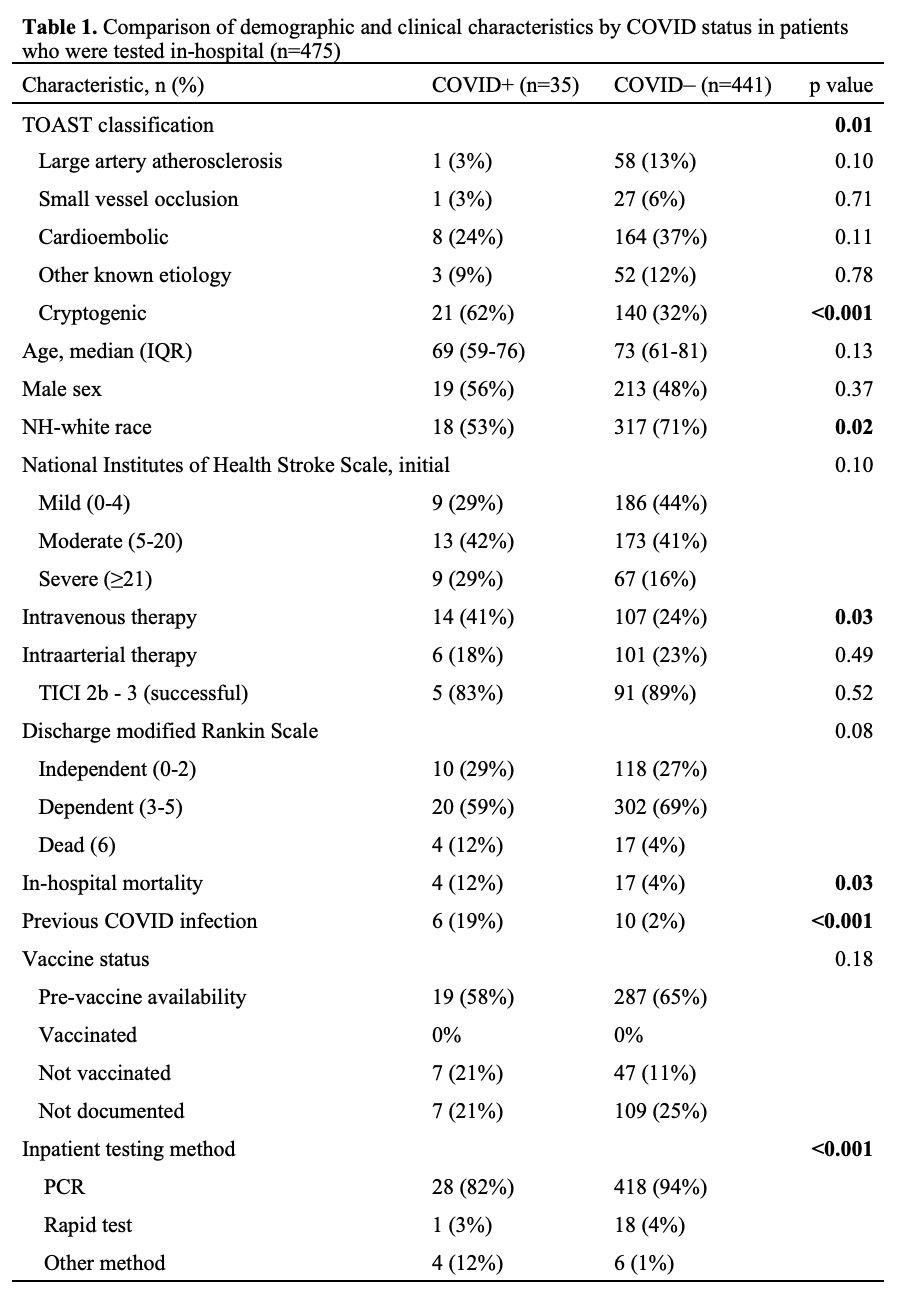
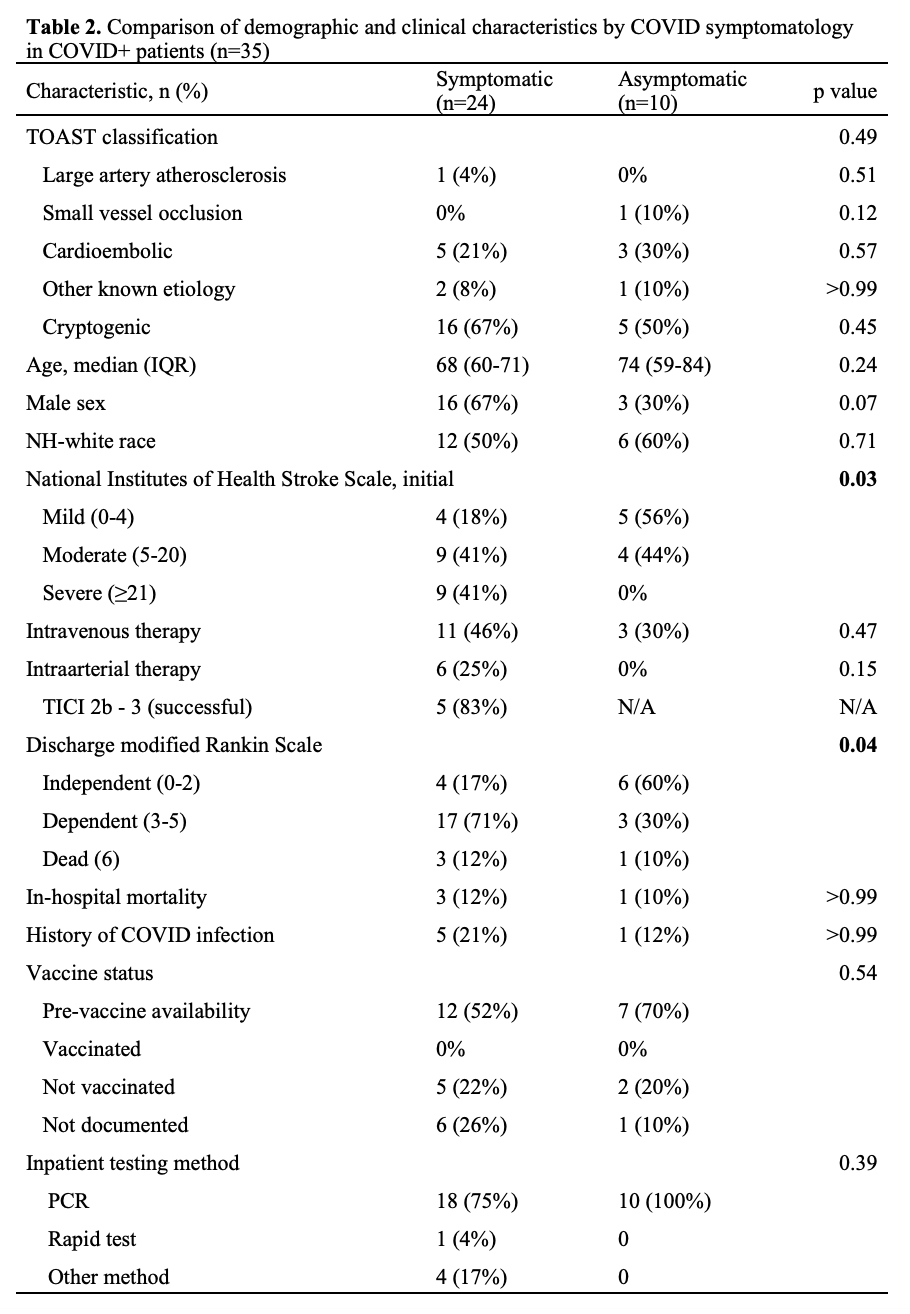
Methods: We retrospectively evaluated adults (≥18) with AIS admitted during the first year of the COVID pandemic (3/1/2020 – 3/1/2021). Demographics (age, sex, race, comorbidities with ≥5% incidence), stroke subtype (TOAST classification), severity (NIHSS), management (intravenous and intraarterial therapy [IVT and IAT]), and outcomes (in-hospital mortality and discharge modified Rankin scale [mRS]) were compared for patients who were COVID+ vs COVID– using Pearson chi-square tests.
Results: Among 1,086 AIS patients, 475 (44%) were evaluated for COVID-19 infection during their inpatient stay. Most patients (94%) had PCR testing. Thirty-five (7%) patients were COVID+ and 441 (93%) were COVID–. There were significant differences in study covariates by COVID status, table 1. COVID+ patients had a greater proportion of cryptogenic strokes (62% vs. 32%, p<0.001), were more likely to report previous COVID infection (19% vs. 2%, p<0.001), were more likely to receive IVT (41% vs. 24%, p=0.03), and were less likely to be non-Hispanic white (53% vs. 71%, p=0.02) compared to COVID– patients. In-hospital mortality was significantly greater in COVID+ versus COVID– patients (12% vs. 4%, p=0.03); however, discharge mRS was not significantly different (p=0.08). When comparing symptomatic (n=10) and asymptomatic (n=24) COVID+ patients, symptomatic patients were more likely to present with severe stroke (NIHSS ≥21: 41% vs. 0%, p=0.03) and worse mRS (independent [0-2]: 17% vs. 60%, p=0.04); there were no other demographic or clinical differences by symptomatology.
Discussion: In the setting of a widespread pandemic such as COVID-19, stroke etiology, severity, and clinical outcomes can differ significantly based on COVID status. These data suggest that patients with AIS and COVID were more likely to have cryptogenic stroke, higher mortality, and, in the case of symptomatic COVID, worse stroke severity and neurologic disability at discharge.
More abstracts on this topic:
Abrams Jessica, Nunes Maria, Diniz Marina, Fraga Lucas, Paula Luiza, Coelho Cecilia, Tacuri Chavez Luz Marina, Lemos Larissa, Correia Julliane, Ribeiro Antonio, Nascimento Bruno, Sable Craig, Spaziani Alison, Zuhlke Liesl, Cardoso Clareci, Vinhal Wanessa, Ribeiro Isabely, Oliveira Kaciane, Amaral Ingred Beatriz
Impaired blood pressure regulation in post-COVID-19 postural orthostatic tachycardia syndrome: novel disease mechanisms beyond sinus tachycardiaJohansson Madeleine, Stahlberg Marcus, Ricci Fabrizio, Lewinter Christian, Hamrefors Viktor, Nilsson Peter, Sutton Richard, Fedorowski Artur
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.