Final ID: WP268
The COVID-19 Pandemic Significantly Affected Acute Ischemic Stroke Subtype, Patient Characteristics, and Outcomes
Abstract Body: Introduction: The overall composition of stroke subtype is typically stable within biogeographical groups. Whether the COVID-19 pandemic impacted stroke etiology is still being investigated, but most studies have been performed outside the United States. This study sought to determine the composition of acute ischemic strokes (AIS) before and during the pandemic.
Methods: This retrospective cohort study was conducted at a comprehensive stroke center in Colorado (USA). Adults (≥18) with AIS were compared based on admission date: Pre-COVID period (1/1/2019 – 12/31/2019) vs. COVID period (3/1/2020 – 3/1/2021). Stroke subtype was examined using TOAST classification: 1) large artery atherosclerosis; 2) cardioembolic; 3) small vessel occlusion; 4) other known etiology (e.g., hematologic disorders or arterial dissection); 5) cryptogenic stroke. Comparisons were made with Pearson chi-square tests.
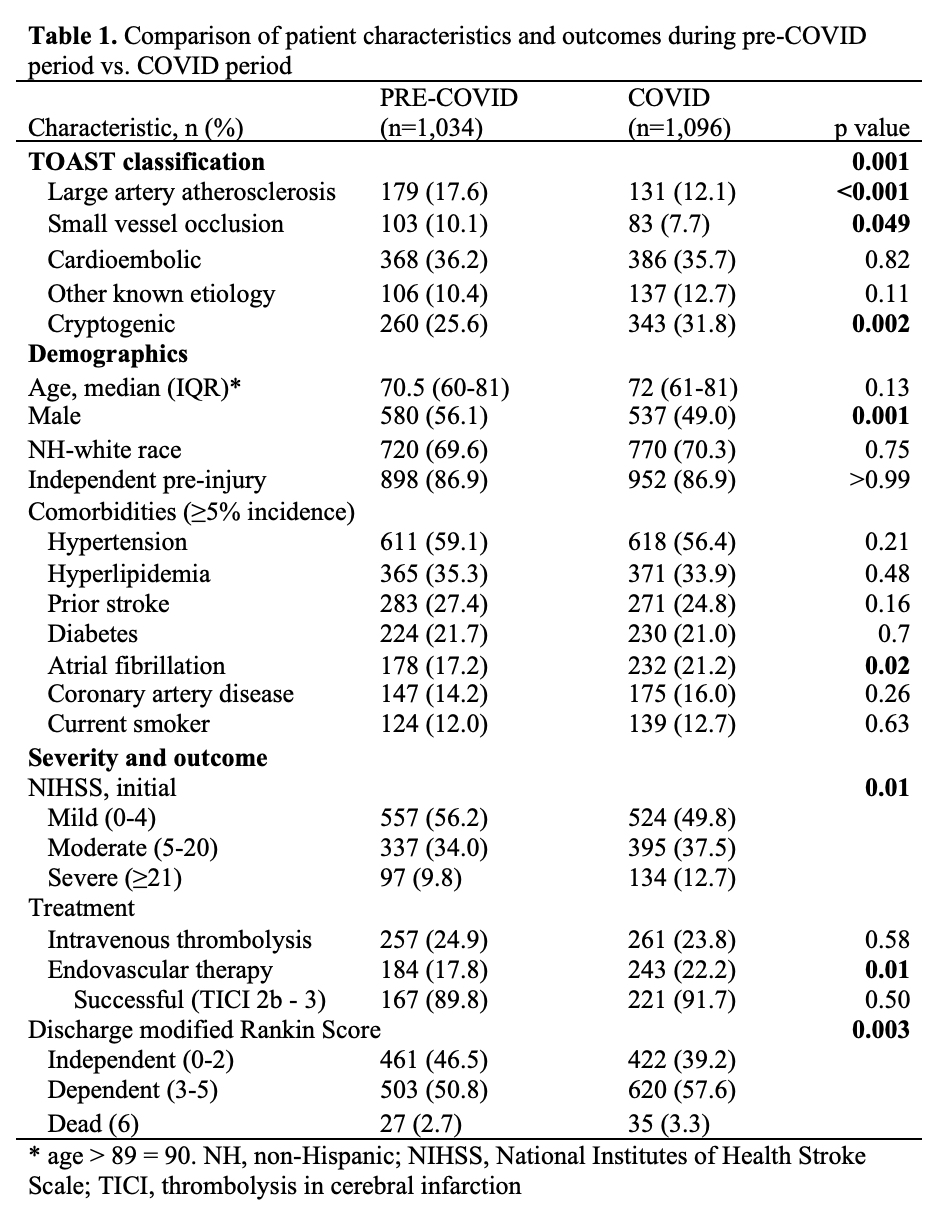
Results: There were 2,130 patients with AIS during the study period: Pre-COVID (n=1,034) and COVID (n=1,096). There were significant differences in stroke subtype by time period (Table 1). Compared to the pre-COVID period, the COVID period had a lower proportion of strokes from large artery atherosclerosis (17.6% vs. 12.1%, p<0.001) and small vessel occlusion (10.1% vs. 7.7%, p=0.05), and significantly more cryptogenic strokes (25.6% vs. 31.8%, p=0.002); rates of cardioembolic stroke and other known etiology were similar between time periods. There were no differences in age, race, and most comorbidities by time period. Compared to the pre-COVID period, there were fewer males (56.1% vs. 49.0%, p=0.001) and more patients with atrial fibrillation (17.2% vs. 21.2%, p=0.02) during the COVID period. Stroke severity and outcomes also differed between time periods. Patients admitted during the COVID period were more likely to be endovascularly treated (17.8% vs. 22.2%, p=0.01), to have more severe strokes (NIHSS ≥21, 9.8% vs. 12.7%, p=0.01), and to have worse discharge mRS compared to patients admitted pre-COVID (Table 1).
Conclusion: In the setting of a widespread pandemic such as COVID-19, stroke etiology, demographics, and clinical outcomes can shift dramatically. These changes included a higher rate of cryptogenic strokes, fewer strokes from large artery atherosclerosis and small vessel occlusion, more strokes among females, a higher number of patients with atrial fibrillation, more patients requiring endovascular treatment, more severe strokes, and worse clinical outcomes.
Methods: This retrospective cohort study was conducted at a comprehensive stroke center in Colorado (USA). Adults (≥18) with AIS were compared based on admission date: Pre-COVID period (1/1/2019 – 12/31/2019) vs. COVID period (3/1/2020 – 3/1/2021). Stroke subtype was examined using TOAST classification: 1) large artery atherosclerosis; 2) cardioembolic; 3) small vessel occlusion; 4) other known etiology (e.g., hematologic disorders or arterial dissection); 5) cryptogenic stroke. Comparisons were made with Pearson chi-square tests.
Results: There were 2,130 patients with AIS during the study period: Pre-COVID (n=1,034) and COVID (n=1,096). There were significant differences in stroke subtype by time period (Table 1). Compared to the pre-COVID period, the COVID period had a lower proportion of strokes from large artery atherosclerosis (17.6% vs. 12.1%, p<0.001) and small vessel occlusion (10.1% vs. 7.7%, p=0.05), and significantly more cryptogenic strokes (25.6% vs. 31.8%, p=0.002); rates of cardioembolic stroke and other known etiology were similar between time periods. There were no differences in age, race, and most comorbidities by time period. Compared to the pre-COVID period, there were fewer males (56.1% vs. 49.0%, p=0.001) and more patients with atrial fibrillation (17.2% vs. 21.2%, p=0.02) during the COVID period. Stroke severity and outcomes also differed between time periods. Patients admitted during the COVID period were more likely to be endovascularly treated (17.8% vs. 22.2%, p=0.01), to have more severe strokes (NIHSS ≥21, 9.8% vs. 12.7%, p=0.01), and to have worse discharge mRS compared to patients admitted pre-COVID (Table 1).
Conclusion: In the setting of a widespread pandemic such as COVID-19, stroke etiology, demographics, and clinical outcomes can shift dramatically. These changes included a higher rate of cryptogenic strokes, fewer strokes from large artery atherosclerosis and small vessel occlusion, more strokes among females, a higher number of patients with atrial fibrillation, more patients requiring endovascular treatment, more severe strokes, and worse clinical outcomes.
More abstracts on this topic:
Post-COVID-19 Patterns of Telehealth Utilization by Cardiovascular Risk Profile in the United States
Johnson Ericka, Parekh Tarang
Association of Estimated Pulse Wave Velocity on Endovascular Treatment Outcome: A Secondary Analysis of the OPTIMAL-BP trialHan Minho, Joo Haram, Lee Hyungwoo, Heo Joonnyung, Jung Jae Wook, Kim Young Dae, Park Eunjeong, Nam Hyo Suk
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)