Final ID: WMP80
Dual Threat - Stroke in Infective Endocarditis: A 10-Year Retrospective Study on Patterns and Predictors of Outcomes
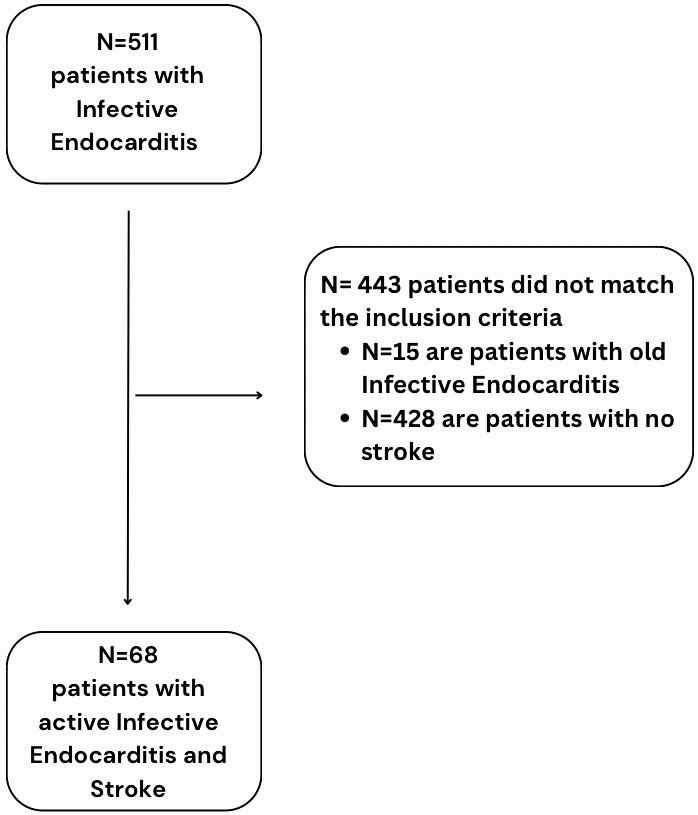
Methods: We conducted a retrospective study of patients diagnosed with infective endocarditis at a single tertiary center over a 10-year period from 2014 to 2023. Out of 526 cases, 511 had active infection and were screened for acute stroke associated with IE. We recorded baseline characteristics including age, gender, comorbidities, echocardiographic findings, vegetation location, microbiological profile, stroke type with radiological features, treatment strategies, and functional outcomes assessed by the Modified Rankin Scale (mRS). Descriptive statistical analysis was performed using IBM SPSS v.20, focusing on predictors of poor outcomes from radiological, microbiological, and echocardiographic data.
Results: Among 511 patients with active IE, 13.3% (68) developed acute stroke, with 80.88% (55) being male. The mitral valve was the most common site for vegetations (66.12%, 41/62). Most cases were culture-negative (39.7%, 27/68), followed by Streptococci (11.76%, 8/68) and Enterococci (10.29%, 7/68). Ischemic strokes accounted for 77.94% of cases, while hemorrhagic strokes occurred in 22.05% (n=68). The middle cerebral artery (MCA) was most frequently affected (54.72%, 29/53). Hemorrhagic transformation was observed in 20.05% of stroke cases. Among hemorrhagic strokes, subdural hemorrhage occurred in 13.3% (2/15) and subarachnoid hemorrhage in 20% (3/15). A favorable outcome (mRS 0-2) was achieved in 41.17% of patients, while 58.82% had poor outcomes (mRS 3-6). The overall mortality rate was 33.82% (23/68), with 69.56% (16/23) of deceased patients having ischemic strokes, often involving the MCA territory (43.76%, 7/16).
Conclusion: Our findings show that patients with ischemic stroke and IE face higher mortality rates. We observed that most strokes occurred in patients with vegetations on native mitral valves. These results emphasize the need for careful monitoring and effective treatment strategies for patients with native valve endocarditis to reduce stroke risk and improve outcomes.
More abstracts on this topic:
Seah Carina, Rivet Dennis, Fraser Justin, Kellner Christopher, Devarajan Alex, Vicari James, Dabney Alan, Baltan Selva, Sohrabji Farida, Pennypacker Keith, Nanda Ashish, Woodward Britton
CCL11 is a pivotal player in the brain-lung axis that mediates stroke outcomes in aged mice with intracerebral hemorrhage.Ozaki Dan, Kitamura Yuki, Bautista-garrido Jesus, Sun Guanghua, Kim Gab Seok, Aronowski Jaroslaw, Jung Joo Eun
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.