Final ID: 40
GENETIC INSIGHTS INTO NOAC THERAPY FAILURE: IMPLICATIONS FOR PRECISION ANTICOAGULATION
Atrial fibrillation (AF) significantly elevates the risk of ischemic stroke and systemic embolism. Novel Oral Anticoagulants (NOACs) have improved stroke prevention in AF, offering superior efficacy and safety compared to warfarin. However, NOAC therapy can fail due to genetic variations, inappropriate dosing, non-adherence, renal dysfunction, hepatic impairment, and drug-drug interactions.This study investigates the potential determinants of NOAC failure, which refers to patients who experienced recurrent thromboembolic events despite being on NOAC therapy.
OBJECTIVES:
To determine the genetic factors (CES1, ABCB1, and ABCG2 polymorphisms) and other contributing factors associated with NOAC therapy failure.
METHODS:
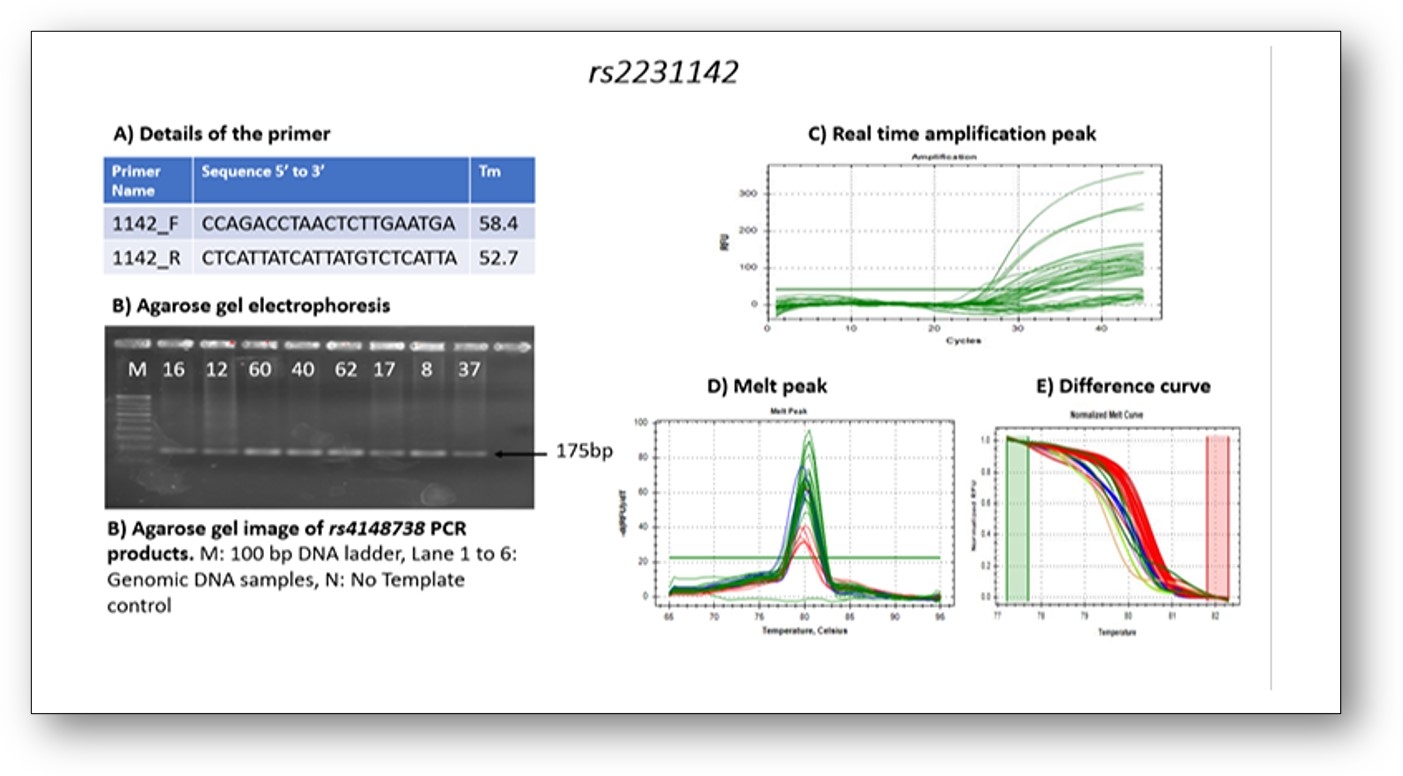
This six-month prospective observational study included adult patients on NOACs for AF, stroke, pulmonary embolism, and other thrombotic events. Exclusions were malignancy and pregnancy/lactation. Data on demographics, medical history, concurrent medications, and clinical outcomes were collected. Genetic polymorphisms were assessed using High-Resolution Melting (HRM)-PCR. Medication adherence was evaluated via the Medication Adherence Rating Scale (MARS), and drug-drug interactions were analyzed using UpToDate software. Statistical analysis was performed using chi-square tests, with a p-value <0.05 considered significant.
RESULTS:
The study included 62 patients (43.5% female, mean age 68 ± 8.9 years). Of these, 46 were on Apixaban, 12 on Dabigatran, and 5 on Rivaroxaban. Recurrent thromboembolic events occurred in 13 (21%) patients within 3.5 months of NOAC initiation. Renal and hepatic impairments had minimal association with NOAC failure; no significant drug-drug interactions were noted. Of the 46 Apixaban users, 17 (37%) carried SNP rs2231142, with 4 (24%) experiencing recurrent events (p=0.039), and 11 (24%) carried SNP rs4148738, with 3 (27%) having recurrent events (p=0.000). For Dabigatran, 4 (33%) carried SNP rs8192935, with 2 (50%) having recurrent events (p=0.083). No polymorphisms were found in Rivaroxaban users.
CONCLUSION:
SNPs rs2231142 and rs4148738 were significantly associated with recurrent thromboembolic events in Apixaban users, suggesting that genetic testing could enhance the prediction of NOAC failure. The findings support the potential role of genetic profiling in optimizing NOAC therapy, given the minimal impact of renal/hepatic impairments and drug-drug interactions.
More abstracts on this topic:
Sen Souvik, Lakshminarayan Kamakshi, Rosamond Wayne, Beck James, Marchesan Julie, Wood Stefanie, Titus Ryan, Moss Kevin, Alonso Alvaro, Soliman Elsayed, Magnani Jared, Johansen Michelle
Elevated International Normalized Ratio Is Inconsistently Associated With Ischemic Stroke Severity and Outcomes for Patients Taking Direct Oral AnticoagulantsLusk Jay, Matsouaka Roland, Xian Ying, Sun Jie-lena, Mac Grory Brian, Schwamm Lee, Smith Eric, Fonarow Gregg, Bhatt Deepak, Saver Jeffrey, Reeves Mathew
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.