Final ID: DP40
Association of Automated Anatomical Vascular Measurements and Procedural Outcomes in Patients undergoing Endovascular Treatment of Stroke
Abstract Body: Introduction. Challenging anatomy and tortuous vessels have been associated with poor outcomes in endovasculat treatment (EVT) of stroke. We aim to examine the relation between intracranial vascular features and EVT outcomes.
Methods. A pre-existing automatic vascular analysis software of vessels on head-and-neck baseline CTA, was adapted to semi-automatically extract the vascular centerline segment from the internal carotid artery (ICA) origin to the thrombus site. Manual intervention was limited to approximate thrombus location placement and side of occlusion. For each vascular segment, the tortuosity index (TI), the overall mean diameter of the entire segment (OMD) and the last 5 mm (diameter at occlusion site) were computed. We defined: first pass effect (FPE: eTICI≥2c at first pass), successful recanalization (mTICI ≥ 2b), excellent recanalization (mTICI ≥ 2c), intracranial hemorrhage (ICH) and symptomatic ICH (sICH).
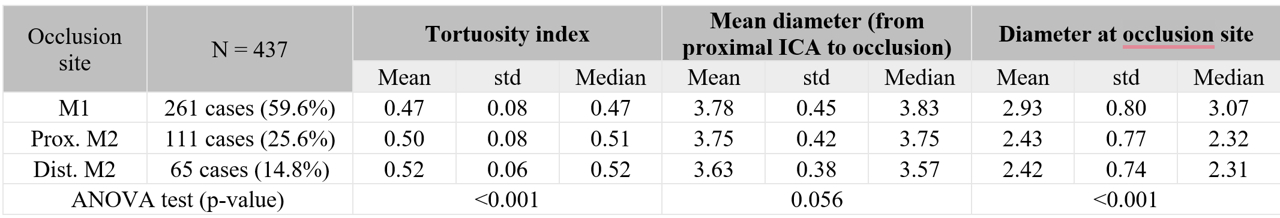
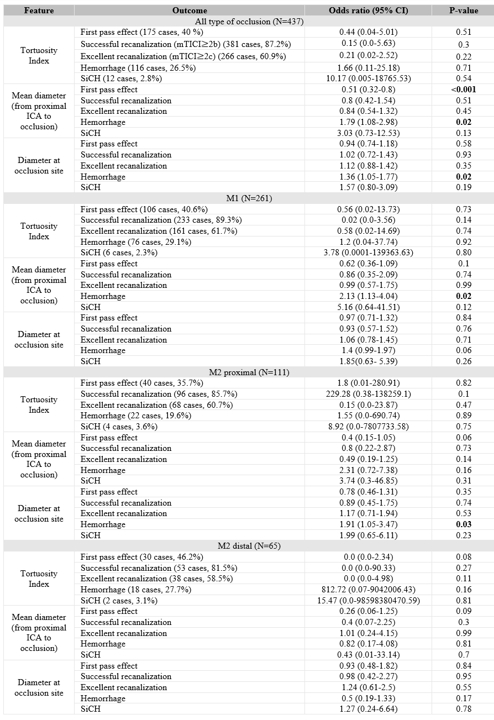
Results: 437 cases with intracranial vessel occlusions in the anterior circulation, treated with EVT between 2017 and 2022 (41% women, median age 81 [IQR 70-88] years), were analyzed (M1: 261 (59.7%); proximal M2: 111(25.4%); M2 distal: 65 (14.9%). Significant differences were found in the diameter at the occlusion site: distal M2: 2.42±0.74mm, proximal M2: 2.43±0.77mm, M1: 2.93±0.80mm (p<0.001) and in the TI: distal M2: 0.52±0.06, proximal M2: 0.50±0.08, M1: 0.47±0.08 (p< 0.001). In the entire population, a larger OMD predicted a lower likelihood of FPE (OR:0.51 (95% CI:0.32-0.80) and a higher risk of ICH (OR:1.79 (95% CI:1.08-2.98). Additionally, a larger diameter at the occlusion site predicted a higher risk of ICH (OR:1.36; 95% CI: 1.05, 1.77) for the entire population and especially for proximal M2 occlusions (OR: 1.91, CI:1.05-3.47).
Conclusions.
Anatomical vascular features automatically extracted from CTA before the procedure can help predict the likelihood of recanalization or the risk of hemorrhagic complications. Further analysis will explore specific anatomical markers that increase the risk of complications, especially in distal occlusions.
Methods. A pre-existing automatic vascular analysis software of vessels on head-and-neck baseline CTA, was adapted to semi-automatically extract the vascular centerline segment from the internal carotid artery (ICA) origin to the thrombus site. Manual intervention was limited to approximate thrombus location placement and side of occlusion. For each vascular segment, the tortuosity index (TI), the overall mean diameter of the entire segment (OMD) and the last 5 mm (diameter at occlusion site) were computed. We defined: first pass effect (FPE: eTICI≥2c at first pass), successful recanalization (mTICI ≥ 2b), excellent recanalization (mTICI ≥ 2c), intracranial hemorrhage (ICH) and symptomatic ICH (sICH).
Results: 437 cases with intracranial vessel occlusions in the anterior circulation, treated with EVT between 2017 and 2022 (41% women, median age 81 [IQR 70-88] years), were analyzed (M1: 261 (59.7%); proximal M2: 111(25.4%); M2 distal: 65 (14.9%). Significant differences were found in the diameter at the occlusion site: distal M2: 2.42±0.74mm, proximal M2: 2.43±0.77mm, M1: 2.93±0.80mm (p<0.001) and in the TI: distal M2: 0.52±0.06, proximal M2: 0.50±0.08, M1: 0.47±0.08 (p< 0.001). In the entire population, a larger OMD predicted a lower likelihood of FPE (OR:0.51 (95% CI:0.32-0.80) and a higher risk of ICH (OR:1.79 (95% CI:1.08-2.98). Additionally, a larger diameter at the occlusion site predicted a higher risk of ICH (OR:1.36; 95% CI: 1.05, 1.77) for the entire population and especially for proximal M2 occlusions (OR: 1.91, CI:1.05-3.47).
Conclusions.
Anatomical vascular features automatically extracted from CTA before the procedure can help predict the likelihood of recanalization or the risk of hemorrhagic complications. Further analysis will explore specific anatomical markers that increase the risk of complications, especially in distal occlusions.
More abstracts on this topic:
A Cross-scale Causal Machine Learning Framework Pinpoints Mgl2+ Macrophage Orchestrators of Balanced Arterial Growth
Han Jonghyeuk, Kong Dasom, Schwarz Erica, Takaesu Felipe, Humphrey Jay, Park Hyun-ji, Davis Michael E
A Deep Learning Topic Analysis Approach for Enhancing Risk Assessment in Heart Failure Using Unstructured Clinical NotesAdejumo Philip, Pedroso Aline, Khera Rohan
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)