Final ID: WP155
Cancer Related Stroke (CRS) in patients with Brain Metastasis; Prevalence and Outcomes.
Abstract Body: Background:
Cancer-related stroke (CRS) is a rare condition where a tumor or its metastasis can compress a blood vessel and result in stroke. Strokes in cancer patients, particularly those with brain metastases, can often be overlooked or misattributed to other causes, making it vital to investigate this association further. In this study, we wanted to see the prevalence of ischemic or hemorrhagic stroke in patients with metastatic cancer to the brain, the demographic characteristics, and associated comorbidities.
Methods:
We conducted a retrospective analysis using the National Inpatient Sample Database from 2016 to 2020. We used ICD-10 codes to diagnose patients with a primary diagnosis of brain metastasis (ICD-10 C7931). Patients were divided into those with strokes (ischemic or hemorrhagic) and those without strokes. We used multivariate analysis to derive the adjusted odds ratio, and all weighted analyses were carried out using STATA.
Results:
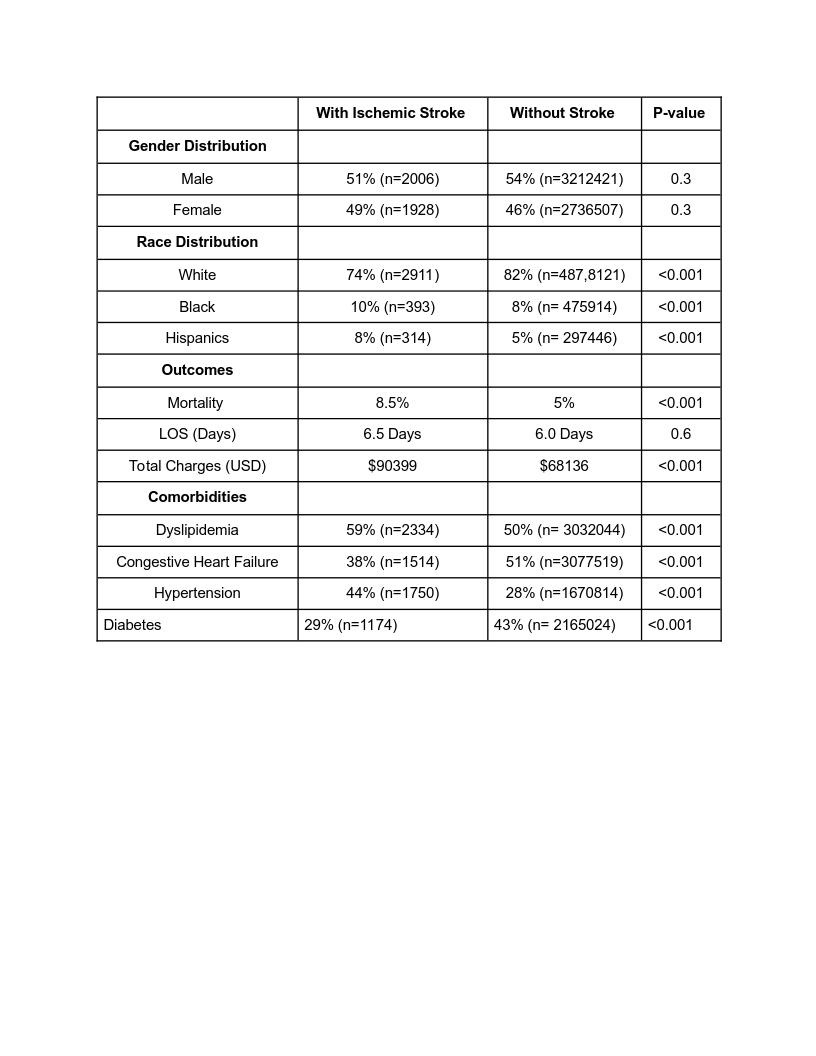
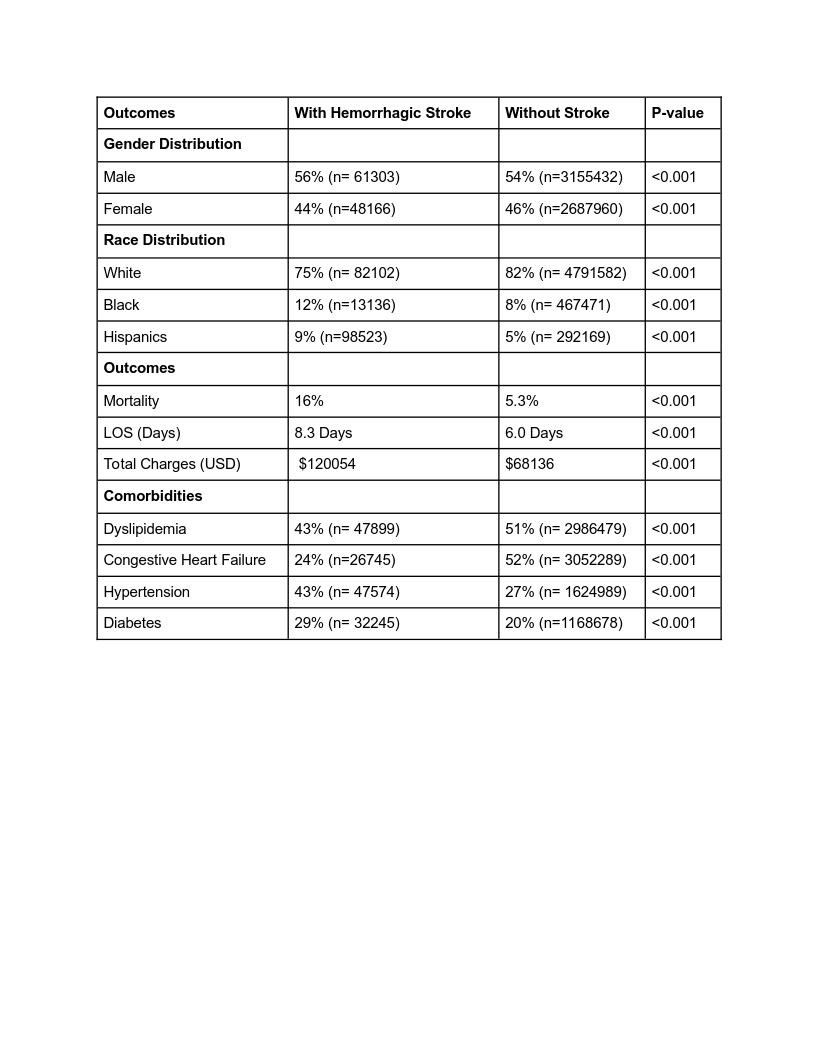
We diagnosed a total of 595,2863 patients with brain metastasis. Out of them, 0.066% (n=3935) patients were found to have ischemic stroke, while 1.8% (n= 109,470) patients had hemorrhagic stroke. For ischemic stroke, the age of the patients was 78 years (p-value 0.01); 49% of the patients were female, while 51% were male (p-value 0.3). For hemorrhagic stroke, the mean age of the patients was 71 years (p-value <0.01); 44% were female, and 56% were male (p-value <0.01). Both types of stroke were most common in the white race (p-value <0.001). The presence of both kinds of stroke was associated with increased mortality in the patients. For ischemic stroke, mortality was 8.5%, aOR 1.7, p-value <0.001, while 16% for hemorrhagic, aOR 3.7, p-value <0.001 for patients with hemorrhagic stroke. The mean length of stay (LOS) was increased in patients with ischemic stroke (6.5 days vs. six days) and hemorrhagic stroke (8.3 days vs six days), along with an increase in total hospital charges (USD) in patients with stroke as compared to those without stroke (Table 1 and 2).
Conclusion:
Our study findings suggest that stroke, both ischemic and hemorrhagic, is associated with increased mortality and more extended hospital stays in this population. These results emphasize the importance of recognizing and addressing the elevated risk of stroke in patients with metastatic cancer to the brain, which can ultimately improve clinical outcomes and patient care.
Cancer-related stroke (CRS) is a rare condition where a tumor or its metastasis can compress a blood vessel and result in stroke. Strokes in cancer patients, particularly those with brain metastases, can often be overlooked or misattributed to other causes, making it vital to investigate this association further. In this study, we wanted to see the prevalence of ischemic or hemorrhagic stroke in patients with metastatic cancer to the brain, the demographic characteristics, and associated comorbidities.
Methods:
We conducted a retrospective analysis using the National Inpatient Sample Database from 2016 to 2020. We used ICD-10 codes to diagnose patients with a primary diagnosis of brain metastasis (ICD-10 C7931). Patients were divided into those with strokes (ischemic or hemorrhagic) and those without strokes. We used multivariate analysis to derive the adjusted odds ratio, and all weighted analyses were carried out using STATA.
Results:
We diagnosed a total of 595,2863 patients with brain metastasis. Out of them, 0.066% (n=3935) patients were found to have ischemic stroke, while 1.8% (n= 109,470) patients had hemorrhagic stroke. For ischemic stroke, the age of the patients was 78 years (p-value 0.01); 49% of the patients were female, while 51% were male (p-value 0.3). For hemorrhagic stroke, the mean age of the patients was 71 years (p-value <0.01); 44% were female, and 56% were male (p-value <0.01). Both types of stroke were most common in the white race (p-value <0.001). The presence of both kinds of stroke was associated with increased mortality in the patients. For ischemic stroke, mortality was 8.5%, aOR 1.7, p-value <0.001, while 16% for hemorrhagic, aOR 3.7, p-value <0.001 for patients with hemorrhagic stroke. The mean length of stay (LOS) was increased in patients with ischemic stroke (6.5 days vs. six days) and hemorrhagic stroke (8.3 days vs six days), along with an increase in total hospital charges (USD) in patients with stroke as compared to those without stroke (Table 1 and 2).
Conclusion:
Our study findings suggest that stroke, both ischemic and hemorrhagic, is associated with increased mortality and more extended hospital stays in this population. These results emphasize the importance of recognizing and addressing the elevated risk of stroke in patients with metastatic cancer to the brain, which can ultimately improve clinical outcomes and patient care.
More abstracts on this topic:
A Rare Case of Acute Undifferentiated Leukemia Presenting as an Isolated Cardiac Mass
Mallipeddi Tarun, Rantanen Petra, Debakey Michael, Cheng Lily, Waheed Nida
ACUTE ISCHEMIC STROKE IN YOUNG CANNABIS USERS: A NATIONWIDE ANALYSISJoseph Varughese Vivek, Anil Peethambar Gowri, Jayaraj Ranjini Nived, Mummadisetty Anvitha
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)