Final ID: TP185
Perihematomal Edema and Hematoma Coagulation a Double-Edged Sword After Acute Spontaneous Intracerebral Hemorrhage (ICH).
Abstract Body: Objective:
To investigate the post-ICH association between the hematoma coagulation and an increase in surrounding perihematomal edema (PHE) volume using serial non-invasive MRI in patients with acute hemorrhagic stroke.
Introduction:
PHE is excessive fluid accumulation encompassing brain swelling, elevated intracranial pressure (ICP), tissue herniation, and midline shift. Typical treatment strategies include decompressive hemicraniectomy and hyperosmolar therapy. Post-ICH release of lysed blood products and other neurotoxins has been associated with PHE growth. However, very little is known about the role of hematoma coagulation in PHE growth. Here, using a recently developed imaging marker of cerebral coagulation, we investigated the relation between the clotted blood volume within hematoma and PHE development.
Methods:
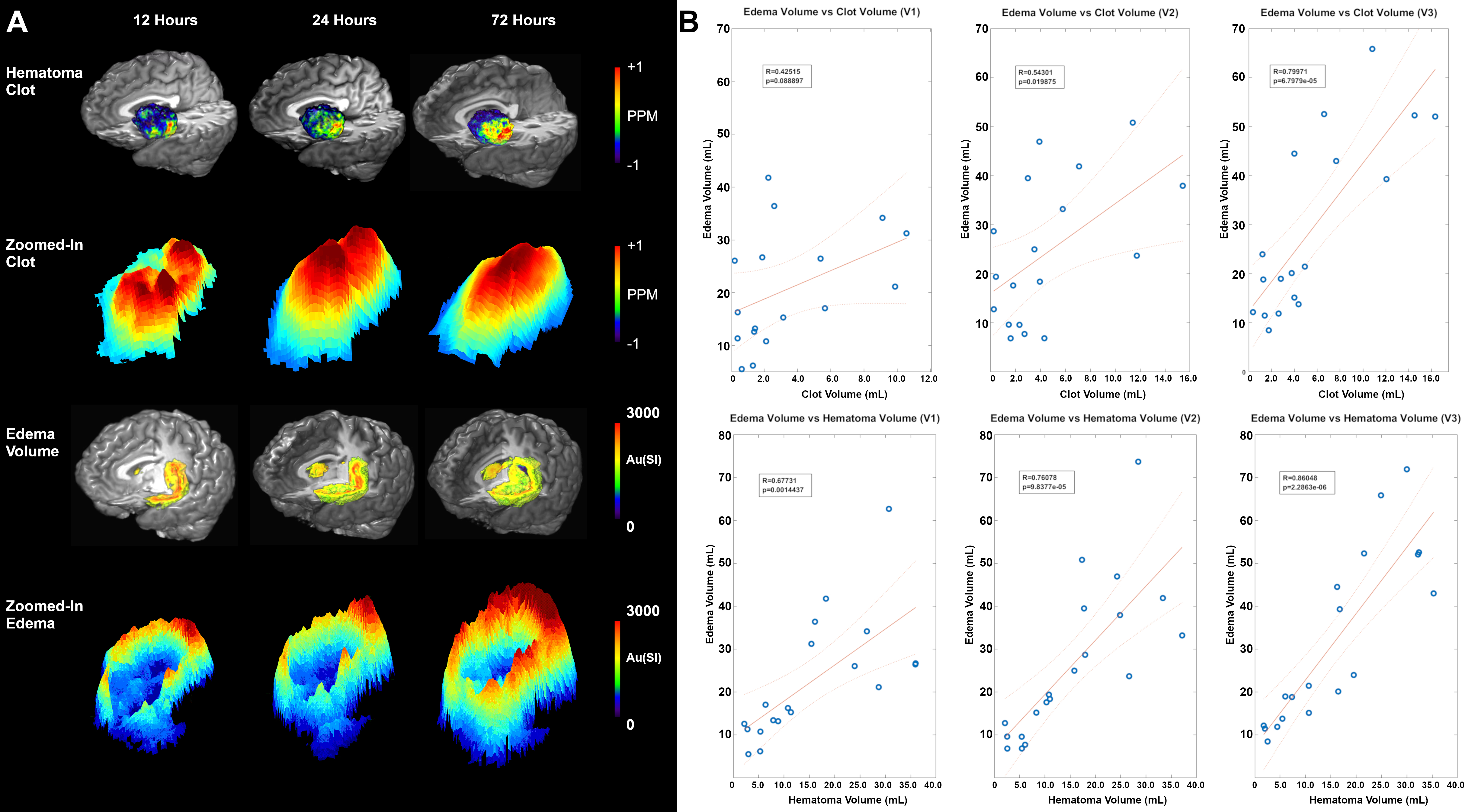
In this retrospective serial MRI image analysis, twenty-four patients with acute spontaneous ICH were imaged 3 times within 12-24 (V1), 36-48 (V2), and 60-72(V3) hours of last seen well (LSW) on a 3T MRI system. 3D anatomical (FLAIR, T1W), multi gradient echo (mGRE), and diffusion tensor (DTI) images were acquired. Using FLAIR images, hematoma and PHE volumes (HV, EV) were segmented and applied as a region of interest (ROI). Quantitative Susceptibility Maps (QSM) and Mean Diffusivity (MD) maps were created using mGRE and DTI images. The HV voxel with susceptibility less and greater than 0.5ppm were categorized as liquid and clotted blood voxel respectively. The clotted blood volume (CBV) was associated with HV, EV, NIHSS, and MD. A non-linear regression model was used for statistical analysis.
Results:
We enrolled 14M/10F, with an average age of 65.8±12y diagnosed with mild spontaneous ICH. Temporally, between the V1 and V3 imaging, the EV (22.9±12.3 to 31.4±19 mL; P<0.05) and CBV (3.36±3.3 to 5.58±4.8 mL; P< 0.05) significantly increased. A significant increase (R=0.42, P = 0.08 to R = 0.80, P < 0.05) positive correlation between EV and CBV was recorded. A positive (P < 0.05) association was also observed between EV and HV whereas no association among MD, NIHSS, and CBV was recorded at any time. These results are summarized in Figure 1.
Conclusion:
Here, we showed hematoma coagulopathy plays a significant role in perihematomal growth in patients with acute ICH. We speculate that the presence of non-coagulated and coagulated blood within the hematoma increases the risk of hematoma and PHE expansion respectively.
To investigate the post-ICH association between the hematoma coagulation and an increase in surrounding perihematomal edema (PHE) volume using serial non-invasive MRI in patients with acute hemorrhagic stroke.
Introduction:
PHE is excessive fluid accumulation encompassing brain swelling, elevated intracranial pressure (ICP), tissue herniation, and midline shift. Typical treatment strategies include decompressive hemicraniectomy and hyperosmolar therapy. Post-ICH release of lysed blood products and other neurotoxins has been associated with PHE growth. However, very little is known about the role of hematoma coagulation in PHE growth. Here, using a recently developed imaging marker of cerebral coagulation, we investigated the relation between the clotted blood volume within hematoma and PHE development.
Methods:
In this retrospective serial MRI image analysis, twenty-four patients with acute spontaneous ICH were imaged 3 times within 12-24 (V1), 36-48 (V2), and 60-72(V3) hours of last seen well (LSW) on a 3T MRI system. 3D anatomical (FLAIR, T1W), multi gradient echo (mGRE), and diffusion tensor (DTI) images were acquired. Using FLAIR images, hematoma and PHE volumes (HV, EV) were segmented and applied as a region of interest (ROI). Quantitative Susceptibility Maps (QSM) and Mean Diffusivity (MD) maps were created using mGRE and DTI images. The HV voxel with susceptibility less and greater than 0.5ppm were categorized as liquid and clotted blood voxel respectively. The clotted blood volume (CBV) was associated with HV, EV, NIHSS, and MD. A non-linear regression model was used for statistical analysis.
Results:
We enrolled 14M/10F, with an average age of 65.8±12y diagnosed with mild spontaneous ICH. Temporally, between the V1 and V3 imaging, the EV (22.9±12.3 to 31.4±19 mL; P<0.05) and CBV (3.36±3.3 to 5.58±4.8 mL; P< 0.05) significantly increased. A significant increase (R=0.42, P = 0.08 to R = 0.80, P < 0.05) positive correlation between EV and CBV was recorded. A positive (P < 0.05) association was also observed between EV and HV whereas no association among MD, NIHSS, and CBV was recorded at any time. These results are summarized in Figure 1.
Conclusion:
Here, we showed hematoma coagulopathy plays a significant role in perihematomal growth in patients with acute ICH. We speculate that the presence of non-coagulated and coagulated blood within the hematoma increases the risk of hematoma and PHE expansion respectively.
More abstracts on this topic:
A Case Report of Cardiac Tamponade due to Mycoplasma Pneumoniae-induced Pericarditis - A Rare Complication of a Commonly seen Bacterial Infection
Patel Vidhi, Maharjan Reeju, Okan Tetyana, Singh Bhupinder, Colasacco Joseph
Building Nucleic Acid-Based Hirudins:Potent, Selective, and Reversible Protease InhibitorsYu Haixiang, Yan Amy, Pitoc George, Garber Susannah, Clancy Jeffrey, Sullenger Bruce
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)