Final ID: 74
ADC-based Infarct Density – Validating a Novel Imaging Biomarker of Functional Outcome after Endovascular Thrombectomy
Abstract Body: Introduction: Endovascular thrombectomy (EVT) dramatically improves clinical outcomes, but the reduction in final infarct volume only accounts for a minority of the treatment effect. There is a need for surrogate imaging biomarkers that more strongly associate with functional outcome, to refine prognostication and facilitate development of EVT-adjuvant neuroprotective therapies. Our group recently developed a straightforward ADC-based metric of post-EVT infarct density (i.e. a measure of infarct severity). We aimed to validate this novel metric in a multicenter study of EVT patients.
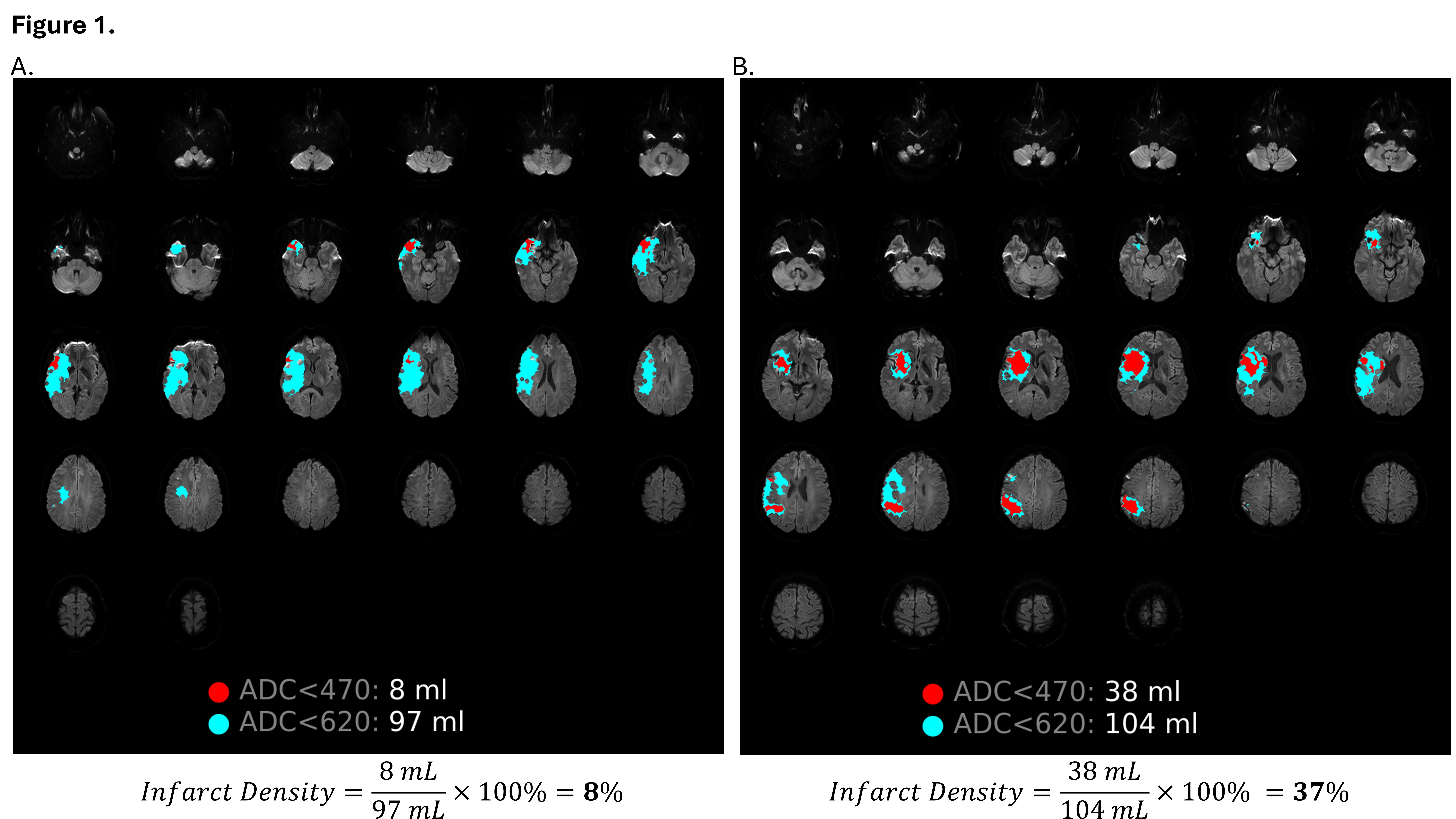
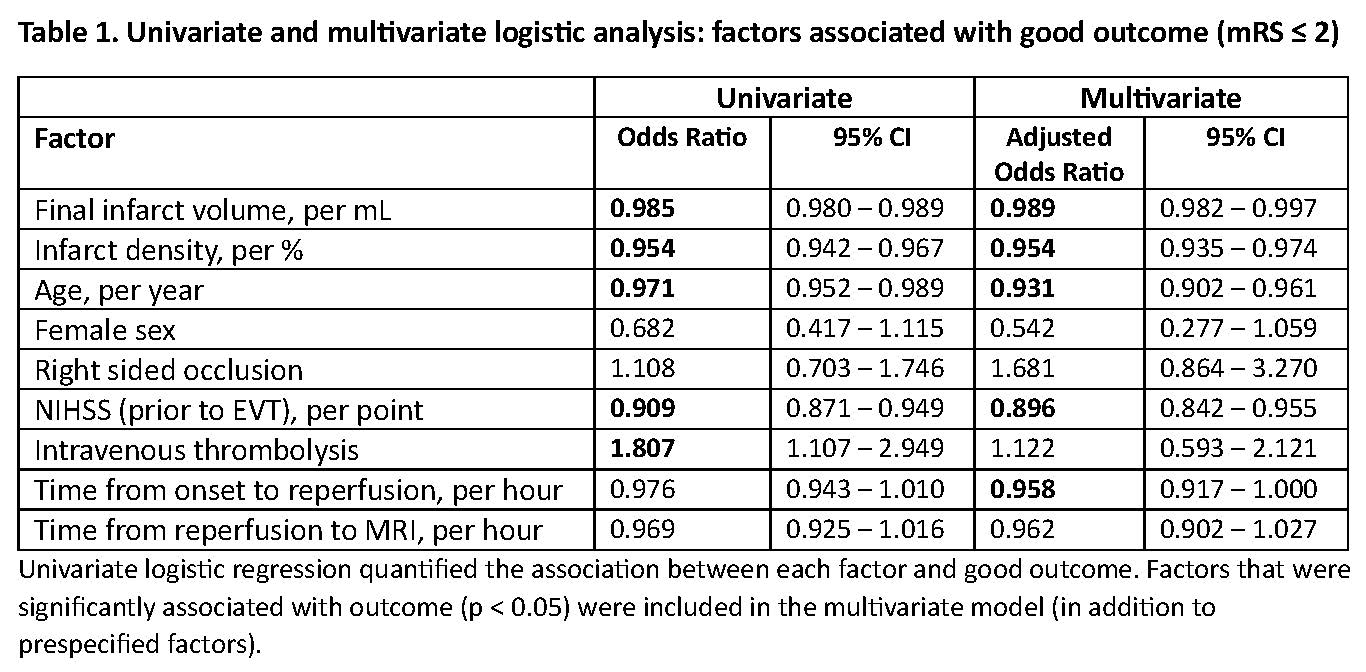
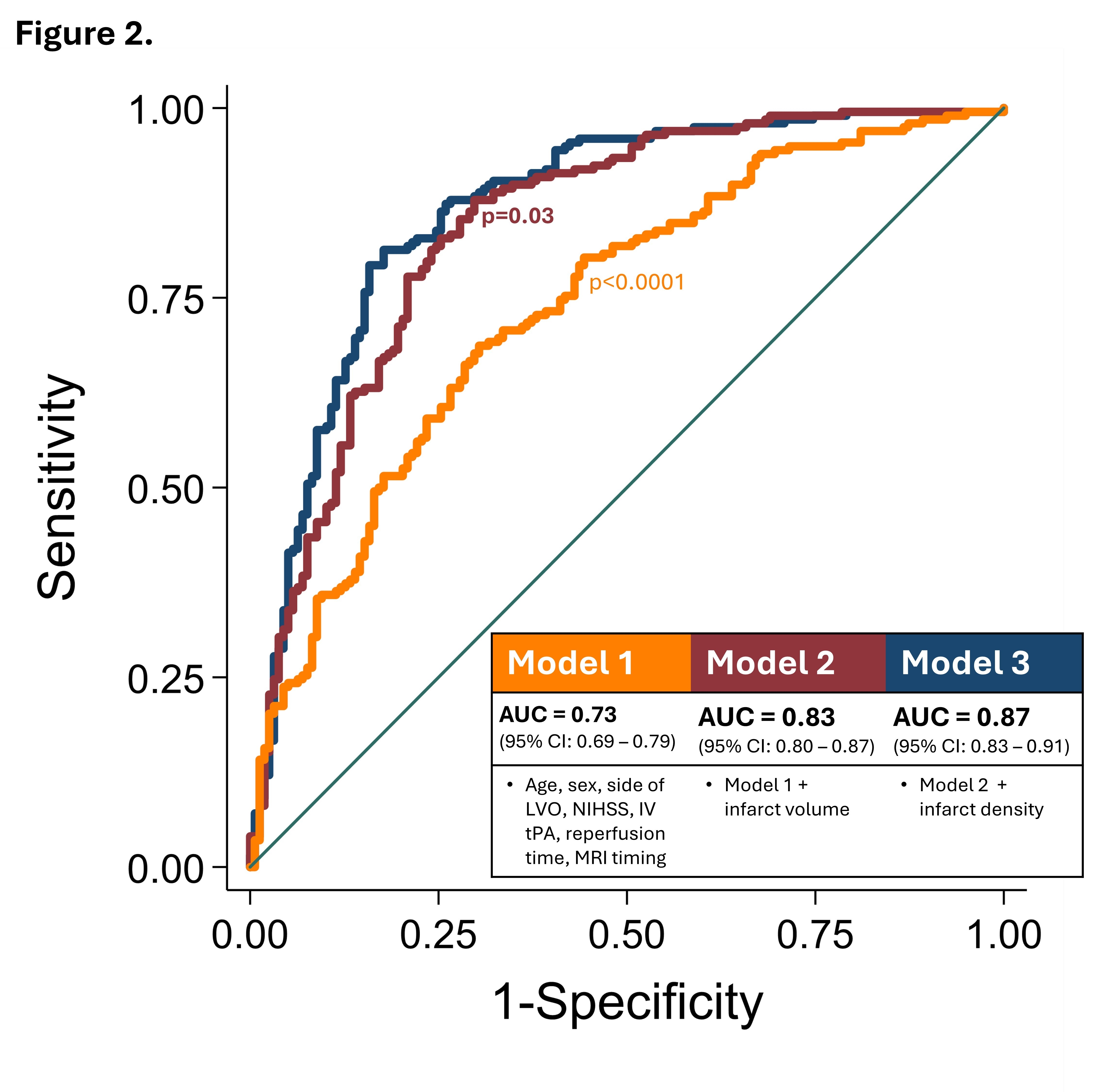
Methods: A retrospective cohort included consecutive patients with anterior circulation LVO who underwent EVT at two stroke centers. MRI was performed 12–48 hours post-EVT. Good functional outcome was defined as a 90-day modified Rankin Scale score ≤2. MR imaging was processed via RAPID, and final infarct volume was based on the standard ADC <620 threshold. Lesion volume was also assessed using ADC <470, and infarct density was calculated as the percentage of final infarct volume with ADC <470 (Figure 1). Multivariate logistic regression quantified the associations between clinical/imaging variables and functional outcome. Model performance was quantified by ROC analysis and compared to a model consisting solely of clinical variables and a model consisting of clinical variables and infarct volume.
Results: Of 312 patients, 284 (92%) achieved successful recanalization (mTICI ≥2b), and 54% achieved a good outcome. The mean age was 69 years (+/- 14); 41% were female. The mean final infarct volume was 50mL (+/- 73). Infarct density was significantly lower in patients with a good outcome (8.3% vs 30.3%, p<0.0001). Table 1 reports the univariate and multivariate analyses. Infarct density was robustly associated with outcome after adjustment for other significant factors including infarct volume (aOR: 0.954 per 1% increase in infarct density). Figure 2 compares the AUC of the three prespecified models, and the best classification was achieved by including infarct density (AUC 0.87; 95%CI: 0.83-0.91).
Conclusion: Infarct density after EVT is independently associated with long term clinical outcome and provides greater prognostic value than final infarct volume alone. Derived from routinely acquired MRI, infarct density is a potentially useful and easily calculable surrogate outcome measure that can be used in clinical trials of EVT-adjuvant therapies.
Methods: A retrospective cohort included consecutive patients with anterior circulation LVO who underwent EVT at two stroke centers. MRI was performed 12–48 hours post-EVT. Good functional outcome was defined as a 90-day modified Rankin Scale score ≤2. MR imaging was processed via RAPID, and final infarct volume was based on the standard ADC <620 threshold. Lesion volume was also assessed using ADC <470, and infarct density was calculated as the percentage of final infarct volume with ADC <470 (Figure 1). Multivariate logistic regression quantified the associations between clinical/imaging variables and functional outcome. Model performance was quantified by ROC analysis and compared to a model consisting solely of clinical variables and a model consisting of clinical variables and infarct volume.
Results: Of 312 patients, 284 (92%) achieved successful recanalization (mTICI ≥2b), and 54% achieved a good outcome. The mean age was 69 years (+/- 14); 41% were female. The mean final infarct volume was 50mL (+/- 73). Infarct density was significantly lower in patients with a good outcome (8.3% vs 30.3%, p<0.0001). Table 1 reports the univariate and multivariate analyses. Infarct density was robustly associated with outcome after adjustment for other significant factors including infarct volume (aOR: 0.954 per 1% increase in infarct density). Figure 2 compares the AUC of the three prespecified models, and the best classification was achieved by including infarct density (AUC 0.87; 95%CI: 0.83-0.91).
Conclusion: Infarct density after EVT is independently associated with long term clinical outcome and provides greater prognostic value than final infarct volume alone. Derived from routinely acquired MRI, infarct density is a potentially useful and easily calculable surrogate outcome measure that can be used in clinical trials of EVT-adjuvant therapies.
More abstracts on this topic:
A Stepwise Approach to Identifying and Assessing the Content Validity of Patient-Reported Outcome (PRO) Measures for Use with Adults with Acute Heart Failure
O'connor Meaghan, Loughlin Anita, Waldman Laura, Rucker Sloan, Vaghela Shailja, Kwon Namhee, Sikirica Vanja
Advanced Complementary Imaging Analysis of Single Ventricle Patients Using Cardiac Magnetic Resonance and EchocardiographyNaum Athanasios, Loke Yue-hin, Meyers Brett, Payne Ronald, Vlachos Pavlos
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)