Final ID: FR415
Tacrolimus-Induced Nephrotoxicity and Hypertensive Urgency in a Renal Transplant Patient: A Case Report
Abstract Body: Case Presentation
A 43-year-old woman with end-stage renal disease (ESRD) due to lupus membranous nephropathy and two renal transplants (most recent in 2018) presented with acute-onset headache, nausea, and vomiting. She was afebrile with blood pressure (BP) 204/123 mmHg and heart rate (HR) 87 bpm. Labs showed blood urea nitrogen (BUN) 63 mg/dL, creatinine 4.44 mg/dL (baseline ~2.5), and urinalysis with 3+ protein and hematuria. Brain MRI/MRA and transplant renal Doppler ultrasound showed no acute pathology. She had no prior hypertension post-transplant and was not on antihypertensives.
Differential Diagnosis
Differentials included tacrolimus-induced hypertension and neurotoxicity, transplant renal artery stenosis, and recurrent glomerulonephritis causing allograft dysfunction.
Treatment and Management
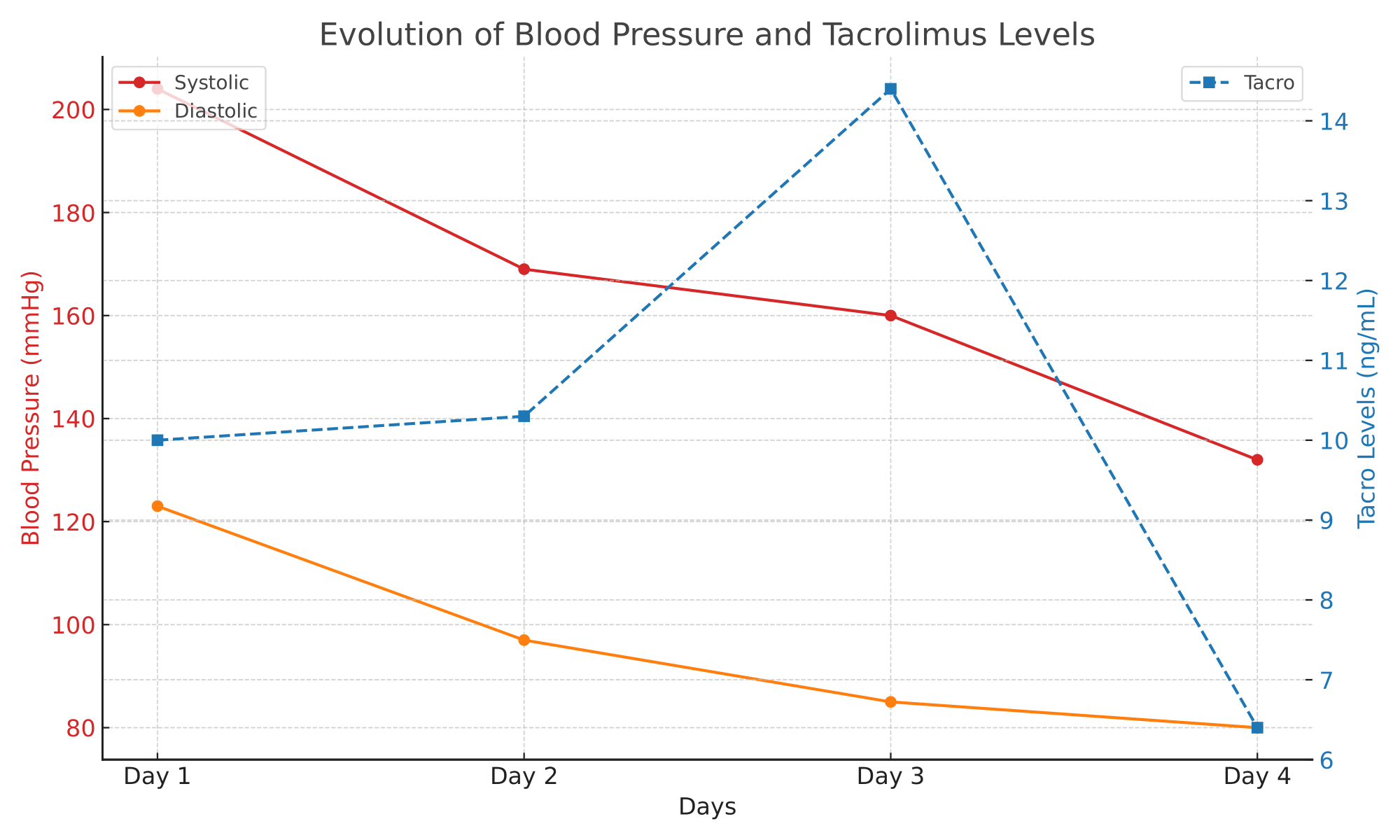
Her immunosuppression included tacrolimus 4 mg AM and 3 mg PM, mycophenolate 180 mg twice daily, and prednisone 5 mg daily. Initial tacrolimus level was 10 ng/mL, rising to 14 ng/mL. Despite carvedilol 6.25 mg twice daily and nifedipine 30 mg daily, BP remained elevated with persistent neurologic symptoms. Neurology ruled out CNS vasculitis by MRI angiography. On hospital day 4, tacrolimus was held due to suspected toxicity. By day 5, BP normalized to 130/80 mmHg, and symptoms resolved (Image 1). She was transitioned to cyclosporine 75 mg twice daily. Renal biopsy was deferred due to prior stability and procedural risk.
Outcomes and Follow-Up
BP stabilized (systolic <130 mmHg) without further medication adjustments. She was discharged with multidisciplinary follow-up for renal replacement therapy and transplant evaluation.
Teaching Point
This case highlights tacrolimus-induced hypertension and neurotoxicity, which can mimic hypertensive urgency or CNS pathology. Tacrolimus causes vasoconstriction and sympathetic activation, and elevated levels may lead to neurotoxic symptoms. Recognition of this mechanism is critical to avoid unnecessary imaging and interventions. Tacrolimus withdrawal resulted in rapid clinical improvement, underscoring the importance of monitoring drug levels and adjusting immunosuppression when toxicity is suspected. Beta-blockers and calcium channel blockers are preferred antihypertensives in transplant recipients due to their complementary mechanisms.
A 43-year-old woman with end-stage renal disease (ESRD) due to lupus membranous nephropathy and two renal transplants (most recent in 2018) presented with acute-onset headache, nausea, and vomiting. She was afebrile with blood pressure (BP) 204/123 mmHg and heart rate (HR) 87 bpm. Labs showed blood urea nitrogen (BUN) 63 mg/dL, creatinine 4.44 mg/dL (baseline ~2.5), and urinalysis with 3+ protein and hematuria. Brain MRI/MRA and transplant renal Doppler ultrasound showed no acute pathology. She had no prior hypertension post-transplant and was not on antihypertensives.
Differential Diagnosis
Differentials included tacrolimus-induced hypertension and neurotoxicity, transplant renal artery stenosis, and recurrent glomerulonephritis causing allograft dysfunction.
Treatment and Management
Her immunosuppression included tacrolimus 4 mg AM and 3 mg PM, mycophenolate 180 mg twice daily, and prednisone 5 mg daily. Initial tacrolimus level was 10 ng/mL, rising to 14 ng/mL. Despite carvedilol 6.25 mg twice daily and nifedipine 30 mg daily, BP remained elevated with persistent neurologic symptoms. Neurology ruled out CNS vasculitis by MRI angiography. On hospital day 4, tacrolimus was held due to suspected toxicity. By day 5, BP normalized to 130/80 mmHg, and symptoms resolved (Image 1). She was transitioned to cyclosporine 75 mg twice daily. Renal biopsy was deferred due to prior stability and procedural risk.
Outcomes and Follow-Up
BP stabilized (systolic <130 mmHg) without further medication adjustments. She was discharged with multidisciplinary follow-up for renal replacement therapy and transplant evaluation.
Teaching Point
This case highlights tacrolimus-induced hypertension and neurotoxicity, which can mimic hypertensive urgency or CNS pathology. Tacrolimus causes vasoconstriction and sympathetic activation, and elevated levels may lead to neurotoxic symptoms. Recognition of this mechanism is critical to avoid unnecessary imaging and interventions. Tacrolimus withdrawal resulted in rapid clinical improvement, underscoring the importance of monitoring drug levels and adjusting immunosuppression when toxicity is suspected. Beta-blockers and calcium channel blockers are preferred antihypertensives in transplant recipients due to their complementary mechanisms.
More abstracts on this topic:
A novel Urocortin-2 analog COR-1167 corrects cardiac and renal dysfunction on top of Empagliflozin in a rat model of acute decompensated heart failure
Stephan Yohan, Corruble Clement, Charrier Lucie, Nicol Lionel, Kowala Mark, Ozoux Marie-laure, Lawson Francesca, Janiak Philip, Mulder Paul
3CPR Best Abstract Award: The pathogenic role of ADAMTS13 deficiency in Chronic Thromboembolic Pulmonary HypertensionWu Zhijian, Zheng X. Long, Zheng Liang