Final ID: FR412
Posterior Reversible Encephalopathy Syndrome (PRES) Complicated With Lacunar Infarcts After Transition To Oral Anti-Hypertensive Medications: A Case Report
Abstract Body: A 48-year-old male presented with sudden diplopia and emesis following 2 weeks of worsening dyspnea, leg edema, and sporadic blurry vision. His personal and family history was unremarkable. Has past tobacco and occasional alcohol use. On arrival, he was afebrile, alert, oriented, with systolic blood pressure (SBP) of 270 mmHg. Neurologic and cardiopulmonary exams were unremarkable. Labs showed renal dysfunction (creatinine 9.53 mg/dL, BUN 99 mg/dL) with unknown baseline, anemia (Hgb 7.1 g/dL), hypokalemia (K 3.1 mmol/L), metabolic acidosis (CO2 18 mmol/L), and elevated troponin (146 ng/L) and BNP (1852 pg/mL).
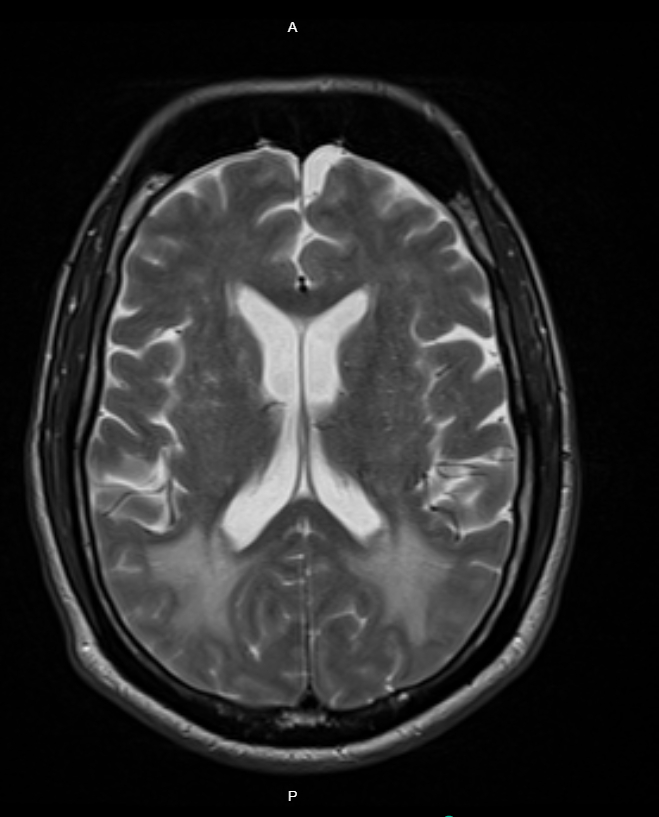
A Head CT showed diffuse white matter hypoattenuation concerning for vasogenic edema or posterior reversible encephalopathy syndrome (PRES). He received 25 mg IV hydralazine and started an IV nicardipine drip, lowering his SBP to 200 mmHg within the first hour and admitted to MICU.
Differential Diagnosis
Initial differentials included PRES and vasogenic edema due to microangiopathy. Reversible cerebral vasoconstriction syndrome (RCVS) was later added based on MRI findings.
Treatment and Management
After 12 hours, Nicardipine was weaned, and oral nifedipine 30 mg started with SBP around 150-180s. Due to SBP spikes of 200 mmHg, nifedipine was increased to 60 mg, and carvedilol 3.125 mg twice daily was added.
Outcome and Follow-Up
After 48 hours, head MRI showed new punctate infarcts consistent with lacunar strokes. MRI Angiography was unremarkable. The patient developed altered mental status, hypotension, and respiratory failure requiring intubation. Repeat CT head showed new right frontal hypoattenuation suggestive of infarction. Antihypertensives were held, and bumetanide drip started for suspected pulmonary edema. After 48 hours, continuous renal replacement therapy was initiated due to worsening renal function. He was extubated on day 5. On day 9, he developed expressive aphasia with preserved strength. He was stabilized and discharged with multidisciplinary follow-up.
Teaching Points
PRES stems from cerebral autoregulation failure and endothelial injury during hypertensive crises. Guidelines recommend gradual BP reduction, but no consensus exists on when to switch IV to oral medication or BP management guidelines past the first 6 hours of a hypertensive crisis. In renal dysfunction, oral drugs may accumulate causing hypotension and reduced cerebral perfusion. This case highlights the risks of early oral transition and the need for evidence-based protocols.
A Head CT showed diffuse white matter hypoattenuation concerning for vasogenic edema or posterior reversible encephalopathy syndrome (PRES). He received 25 mg IV hydralazine and started an IV nicardipine drip, lowering his SBP to 200 mmHg within the first hour and admitted to MICU.
Differential Diagnosis
Initial differentials included PRES and vasogenic edema due to microangiopathy. Reversible cerebral vasoconstriction syndrome (RCVS) was later added based on MRI findings.
Treatment and Management
After 12 hours, Nicardipine was weaned, and oral nifedipine 30 mg started with SBP around 150-180s. Due to SBP spikes of 200 mmHg, nifedipine was increased to 60 mg, and carvedilol 3.125 mg twice daily was added.
Outcome and Follow-Up
After 48 hours, head MRI showed new punctate infarcts consistent with lacunar strokes. MRI Angiography was unremarkable. The patient developed altered mental status, hypotension, and respiratory failure requiring intubation. Repeat CT head showed new right frontal hypoattenuation suggestive of infarction. Antihypertensives were held, and bumetanide drip started for suspected pulmonary edema. After 48 hours, continuous renal replacement therapy was initiated due to worsening renal function. He was extubated on day 5. On day 9, he developed expressive aphasia with preserved strength. He was stabilized and discharged with multidisciplinary follow-up.
Teaching Points
PRES stems from cerebral autoregulation failure and endothelial injury during hypertensive crises. Guidelines recommend gradual BP reduction, but no consensus exists on when to switch IV to oral medication or BP management guidelines past the first 6 hours of a hypertensive crisis. In renal dysfunction, oral drugs may accumulate causing hypotension and reduced cerebral perfusion. This case highlights the risks of early oral transition and the need for evidence-based protocols.
More abstracts on this topic:
Association Between Antiphospholipid Antibody and Ischemic Stroke: A Systematic Review and Meta-Analysis
Watson Nathan, Kanthi Yogen, Secemsky Eric, Connors Jean, Barnes Geoffrey, Goldhaber Samuel, Weitz Jeffrey, Costenbader Karen, Piazza Gregory, Krumholz Harlan, Cushman Mary, Bukhari Syed, Bikdeli Behnood, Rashedi Sina, Weber Brittany, Anderson Christopher, Elkind Mitchell, Pfeferman Mariana, Ujueta Francisco, Zarghami Mehrdad
A durable reduction in blood pressure by ultrasound renal denervation: A real-world, single center experienceKing Jordan, Gharib Wissam