Final ID: TH142
Posterior Reversible Encephalopathy Syndrome: A Diagnostic Challenge and the Critical Role of Blood Pressure Control
Abstract Body: Background:
Posterior Reversible Encephalopathy Syndrome (PRES) is a neurotoxic state characterized by seizures, encephalopathy, visual disturbances, and radiologic findings of vasogenic edema. Etiologies could be divided into clinical conditions (Arterial Hypertension) and toxics (Antineoplastic or Illicit drugs). Recent studies estimate the annual incidence of PRES in the United States at approximately 3 cases per 100,000 individuals, with higher rates observed in women and black individuals.
Case Presentation:
A 47-year-old female with no significant past medical history presented with acute confusion and unresponsiveness. Shortly after arrival to the ED, she had a witnessed generalized tonic-clonic seizure. Postictally, she remained unresponsive with extensor posturing. Initial CT head revealed bilateral occipital and temporal lobe hypodensities concerning for cerebral edema. She received IV midazolam, was loaded with levetiracetam and continuous EEG was initiated to evaluate for nonconvulsive status.
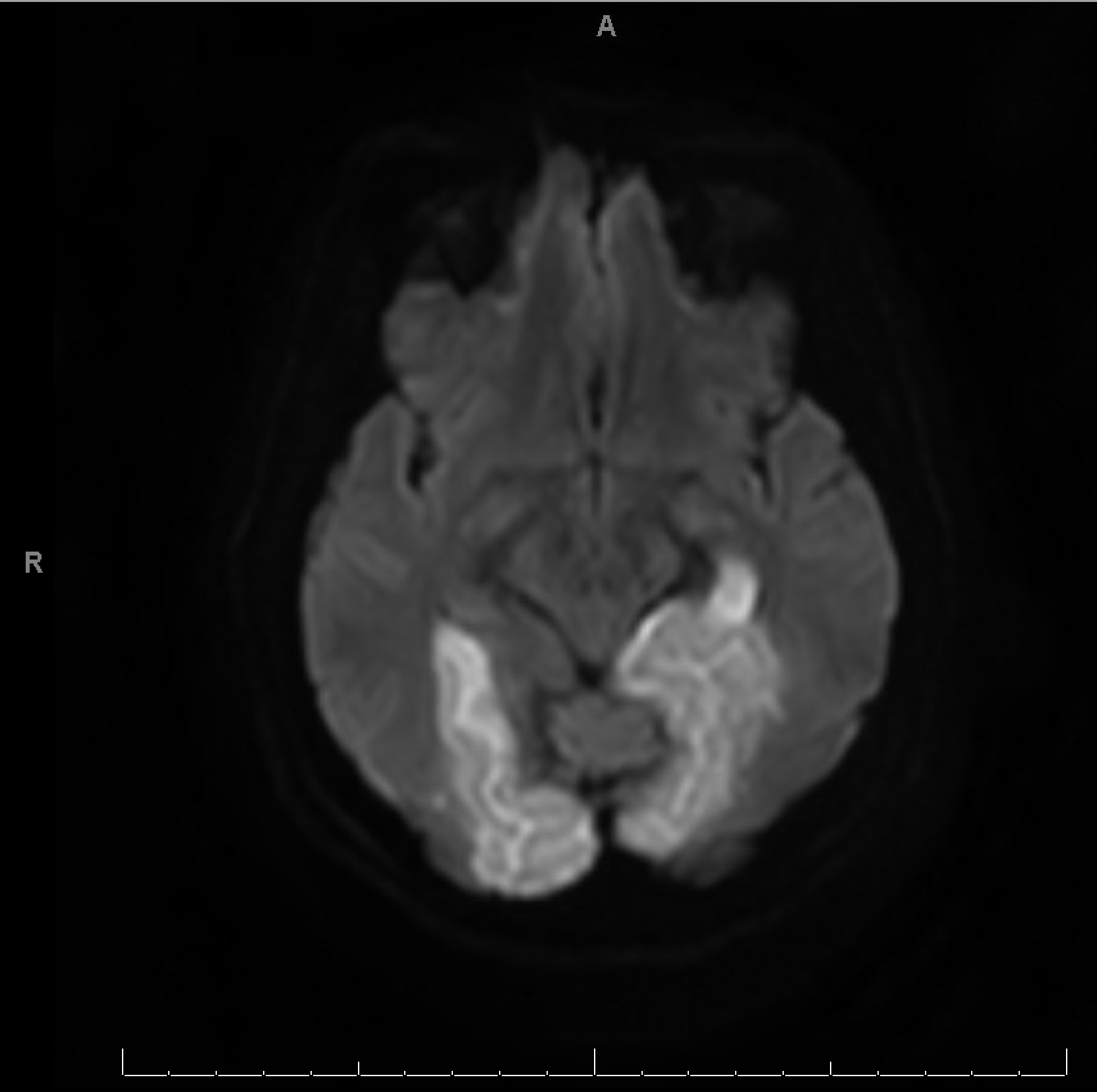
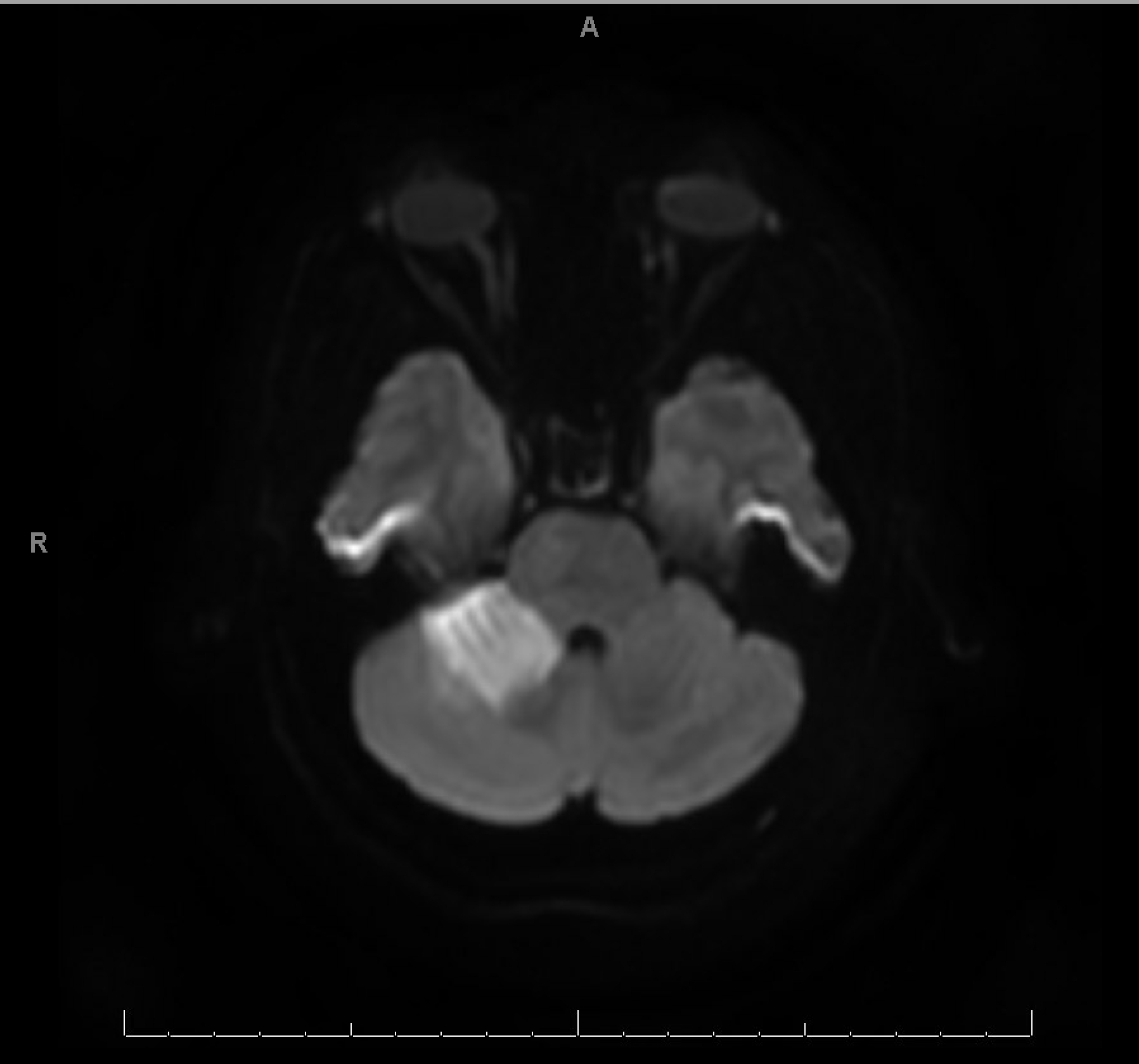
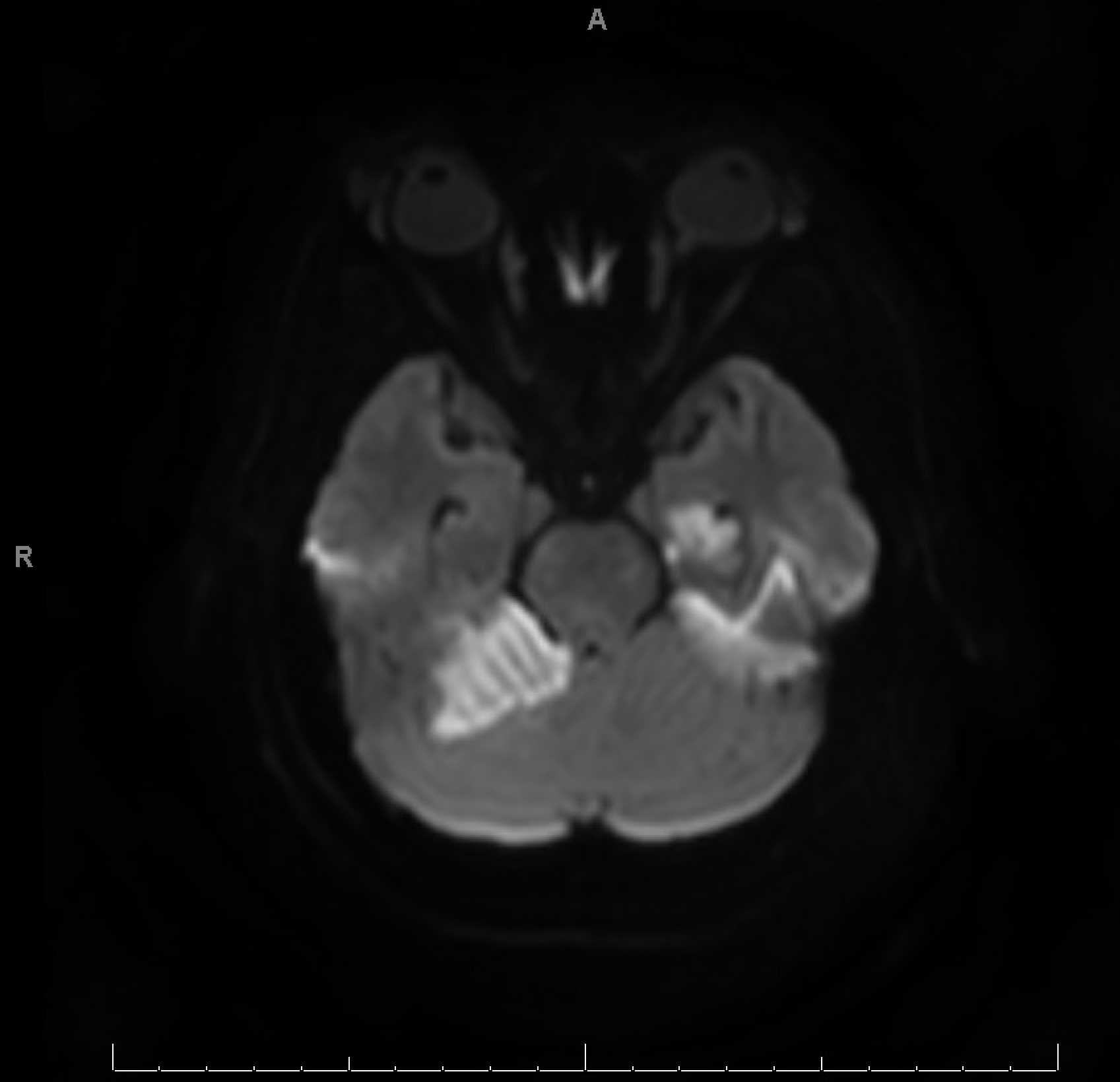
CTA revealed bilateral PCA stenosis, likely due to vasospasm. MRI brain showed bilateral occipital, left mesial temporal, and right cerebellar vasogenic edema with areas of restricted diffusion and microhemorrhages, supporting the diagnosis of PRES. Workup for infection, vasculitis, and autoimmune encephalitis was negative. Hypertensive emergency was suspected as the precipitating factor.
She was managed in the ICU with strict BP control and seizure prophylaxis. LP was deferred due to initial elevated ICP risk and improving clinical course. Over the next few days, her neurological status gradually improved, repeat imaging showed stable findings without new infarcts or hemorrhages. She was discharged on oral antihypertensives and levetiracetam, with plans for close outpatient neurology follow-up, repeat MRI, and cognitive evaluation.
Discussion:
This case underscores the diagnostic complexity of PRES, which can mimic stroke, infection, or structural lesions. Imaging, particularly MRI, is pivotal in distinguishing PRES from infarction. The presence of seizures, encephalopathy, and visual disturbances in the setting of malignant hypertension should prompt immediate consideration of PRES, especially when imaging suggests posterior white matter involvement. This case highlights the urgency of BP control and the need for a multidisciplinary approach, including neurology, radiology, and critical care, to prevent long-term neurological sequelae.
Posterior Reversible Encephalopathy Syndrome (PRES) is a neurotoxic state characterized by seizures, encephalopathy, visual disturbances, and radiologic findings of vasogenic edema. Etiologies could be divided into clinical conditions (Arterial Hypertension) and toxics (Antineoplastic or Illicit drugs). Recent studies estimate the annual incidence of PRES in the United States at approximately 3 cases per 100,000 individuals, with higher rates observed in women and black individuals.
Case Presentation:
A 47-year-old female with no significant past medical history presented with acute confusion and unresponsiveness. Shortly after arrival to the ED, she had a witnessed generalized tonic-clonic seizure. Postictally, she remained unresponsive with extensor posturing. Initial CT head revealed bilateral occipital and temporal lobe hypodensities concerning for cerebral edema. She received IV midazolam, was loaded with levetiracetam and continuous EEG was initiated to evaluate for nonconvulsive status.
CTA revealed bilateral PCA stenosis, likely due to vasospasm. MRI brain showed bilateral occipital, left mesial temporal, and right cerebellar vasogenic edema with areas of restricted diffusion and microhemorrhages, supporting the diagnosis of PRES. Workup for infection, vasculitis, and autoimmune encephalitis was negative. Hypertensive emergency was suspected as the precipitating factor.
She was managed in the ICU with strict BP control and seizure prophylaxis. LP was deferred due to initial elevated ICP risk and improving clinical course. Over the next few days, her neurological status gradually improved, repeat imaging showed stable findings without new infarcts or hemorrhages. She was discharged on oral antihypertensives and levetiracetam, with plans for close outpatient neurology follow-up, repeat MRI, and cognitive evaluation.
Discussion:
This case underscores the diagnostic complexity of PRES, which can mimic stroke, infection, or structural lesions. Imaging, particularly MRI, is pivotal in distinguishing PRES from infarction. The presence of seizures, encephalopathy, and visual disturbances in the setting of malignant hypertension should prompt immediate consideration of PRES, especially when imaging suggests posterior white matter involvement. This case highlights the urgency of BP control and the need for a multidisciplinary approach, including neurology, radiology, and critical care, to prevent long-term neurological sequelae.
More abstracts on this topic:
Atrial Fibrillation and Risk of Incident Cognitive Impairment: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study
Le Vinh, Wilkinson Katherine, Judd Suzanne, Soliman Elsayed, Hyacinth Hyacinth I., Olson Nels, Smith Melissa, Cushman Mary
Association between SGLT2 inhibitors and risk of Dementia and Parkinson’s Disease: A Meta-analysis of 12 Randomized Controlled Trials.Jaiswal Vikash, Mashkoor Yusra, Jaiswal Akash, Raj Nishchita, Rajak Kripa, Fonarow Gregg